Toll Free No.: 1800 2330 0007 email: admin@dhanwantari.com

Diagnostic Tests
Hematological Tests
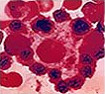
Blood is connective tissue. It circulates in closed blood vessels in the system. The circulating blood consists of erythrocytes (red blood cells), leucocytes (white blood cells), and platelets or thrombocytes in a pale yellow colored fluid called plasma. When blood is given to a pathological lab for routine check up of blood CBC – a complete blood count is performed.

Hemoglobin Determination
It is performed generally by two methods, Sahli method or the Cyanmethemoglobin method:
| Normal Values | Hb, g/dl |
| Men | 14 – 18 |
| Women | 11.5 – 16.5 |
| Children (up to 1 year) | 11.0 – 13.0 |
| Children (10 – 12 years) | 11.5 – 14.5 |
| Infants (full term cord blood) | 3.5 – 19.5 |
 |
Decrease in hemoglobin below the normal range indicates anemia. | |
 |
It also drops in pregnancy due to hemodilution. | |
 |
An increase is also seen in congenital heart disease due to reduced oxygen supply. | |
 |
An increase in hemoglobin in emphysema. | |
 |
An increase in hemoglobin in polycythemia. |
Total Erythrocyte (Red Blood Cells) Count
Normal values:
 |
Male – 4.5 to 6.0 x 106 cells/cu mm (ml) | |
 |
Female – 4.0 to 4.5 x 106 cells/cu mm (ml) | |
 |
At birth – 6.5 to7.25 x 106 cells/cu mm (ml) | |
 |
A decrease in RBC count as also observed in old age, in pregnancy and in diseases which cause anemia. | |
 |
An increase in the RBC count is observed in burns and cholera due to fluid loss. | |
 |
An increase in the RBC count is also observed in chronic heart disease, emphysema and polycythemia. | |
 |
Sometimes, false low counts can be due to edema, an error in calculation or due to improper dilution by the technician. | |
 |
Sometimes, false high counts can be due to hemoconcentration, an error in calculation or due to an improper technique used by the technician. |
Total Leucocyte (White Blood Cells) Count
Normal values:
| Adults | 4,000 – 10,000/cu mm (ml). |
| At birth | 10,000 – 25,000/cu mm (ml). |
| 1 to 3 years | 6,000 – 18,000/cu mm (ml). |
| 4 to 7 years | 6,000 – 15,000/cu mm (ml). |
| 8 to 12 years | 4,500 – 13,500/cu mm (ml). |
If there is an increase in the total WBC count and it is more than 10,000/cu mm (ml), it is known as leucocytosis.

Causes of Leucocytosis:
| 1. | Pathological:
|
||||||||||||||||
| 2. | Physiological:
|
Causes of Leucopenia:
| 1. | Bacterial infections like typhoid, paratyphoid, tuberculosis etc. reduces the count. | |
| 2. | Viral infections like hepatitis, influenza, and measles also reduce the count. | |
| 3. | Protozoal infections like malaria reduce the count. | |
| 4. | Leukemia does it too. | |
| 5. | Primary bone marrow depression (aplastic anemia). | |
| 6. | Secondary bone marrow depression (due to drugs, radiation etc.). | |
| 7. | Anemia (iron deficiency, megaloblastic etc.) |
If there is a decrease in WBC count and it falls to less than 4,000/cu mm (ml), it is known as leucopenia.
Platelets Count
Platelets are very small in diameter – around 3 mm. They help in clotting of blood. Normal platelet count is 250,000 to 500,000/cu mm (ml) and it is said to be adequate. If it is less than that, it is said to be inadequate.
Abnormalities of Erythrocytes (RBC)
In various types of anemia and in other diseases such as thalassemia, malaria, kidney failure etc., the mature RBCs show significant changes. Various changed RBCs seen are termed as microcytes, macrocytes, hypochromic, spherocytes, target cells, stomatocytes, anisocytosis, poilkilocytosis, sickle cells, ovalocytes, elliptocytes, acanthocytes, burr cells, siderocytes, basophilic stippling, howell–jolly body, cobot ring, schi stocytes, crescent bodies and creneted cells depending upon their morphology.
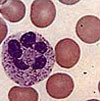
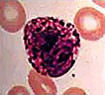
Differential WBC Count
There are five different kinds of WBCs:
| Normal Values | (Male or Female) |
| Neutrophils | 40 – 75% |
| Eosinophils | 1 – 4% |
| Basophils | 0 – 1% |
| Lymphocytes | 20 – 45% |
| Monocytes | 2 – 8% |

|
|

|
Significance of the WBC Count
| A. | When there is an increase in eosinophils it is known as eosinophilia. It is observed in chronic inflammatory conditions, asthma, parasitic infestations, and in hypersensitivity reactions. | ||||||||||||||||||||||
| B. | When there is a decrease in lymphocytes, it is known as lymphopenia. It is observed in acute stages of infections and where there is an excessive irradiation. | ||||||||||||||||||||||
| C. | When there is an increase in neutrophils, it is known as neutrophilia. The common cause is pyogenic (pus forming) bacterial infections. When there is a decrease in neutrophils it is known as neutropenia. It is observed in bacterial infections such as typhoid, viral infection such as measles, influenza etc. It is also found in anemias (aplastic, megaloblastic, iron deficiency) and in suppression of bone marrow by various drugs and radiation. | ||||||||||||||||||||||
| D. |
When there is an increase in lymphocytes it is known as lymphocytosis. Lymphocytosis can be of two types, relative or absolute.
|
||||||||||||||||||||||
| E. | When there is an increase in the number of monocytes, it is known as monocytosis. It is observed in tuberculosis, malaria, sub–acute bacterial endocarditis, typhoid and in Kala Azar. | ||||||||||||||||||||||
| F. | A differential count is useful in identifying changes in the distribution of WBCs, which may be related to specific types of disorders. It also helps to know the severity of the disease and the degree of the response of the body. |
Abnormalities of Leucocytes (WBC)
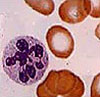
Most abnormalities are seen in Neutrophils. Different WBCs having abnormalities are termed as myelocytes, promyelocytes, blasts, metamyelocytes, plasma cell, smudge cells etc.
Packed Cell Volume (PCV)
PCV (packed cell volume) is the amount of packed red blood cells after centrifugation. It is expressed in the percentage of total blood volume.
Normal values:
| Male | 42–52%. |
| Female | 36–48%. |
| Late pregnancy | 23–37%. |
Increase in PCV is due to polycythemia, dehydration, emphysema, and congenital heart disease. Decrease in PCV is due to different types of anemia, hydremia (excessive fluid in the blood which occurs in pregnancy).
Mean Corpuscular Volume (MCV)
MCV – Mean Cell Volume
 |
Normal value: 82–92 cu mm. | |
 |
Increased MCV indicates macrocytic anemias. | |
 |
Decreased MCV indicates microcytic anemias. |
Mean Corpuscular Hemoglobin (MCH)
MCH – Mean Cell hemoglobin
 |
Normal value: 27–32 pg (pg = 1 picogram = 10–12 g). | |
 |
Increased value indicates macrocytic anemia. | |
 |
Decreased value indicates hypochromia. |
It is average amount of hemoglobin in the red cell compared to normal.
 |
Normal color index: 0.85–1.15. | |
 |
Increase in the color index indicates megaloblastic anemias. | |
 |
Decrease in the color index indicates hypochromic anemia. |
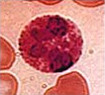
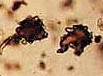
Parasites
Blood parasites cause a number of ailments which are more prevalent in tropical counties. The common diseases caused are malaria, kala azar and sleeping sickness.

The parasites found are:
| A. |
The following parasites cause malaria
|
|||||||||||||||||||
| B. |
The following parasites cause visceral leishmaniasis, dumdum fever or kala azar
|
|||||||||||||||||||
| C. |
The following parasites cause African sleeping sickness
|
|||||||||||||||||||
| D. |
The following parasites cause filaria
|
Mean Corpuscular Hemoglobin Concentration (MCHC)
Normal Value: 32–36%.
 |
Increased value indicates spherocytosis. | |
 |
Decreased value indicates hypochromic anemias. |
Tabular Representation of Normal Values
Blood Routine – Normal Values
| Test | Normal Values | |
| Hemoglobin | Men | 13.5–17.5% |
| Women | 11.5–16.5% | |
| Total WBC Count | Adults: 4000–11000/cu.mm | |
| Differential Count | Neutrophils | 40–75% |
| Eosinophils | 1–6% | |
| Lymphocytes | 20–45% | |
| Monocytes | 2–10% | |
| Basophils | 0–1% | |
| ESR: (Westegren): 1 hr | Men | 1–10 mm |
| Women | 5–15 mm | |
| Platelet Count | 1.5–4.0 lakhs/cu.mm | |
| Reticulocyte Count | Adults: 0.2–2% | |
| RBC (Erythrocyte) Count | Men | 4.5–6.5 million/cu.mm |
| Women | 3.8–5.8 million/cu.mm | |
| Mean Corpuscular Volume | 75–97 fl | |
| Mean Corpuscular Hemoglobin | 26–33 pg | |
| Mean Corpuscular Hemoglobin Concentration | 32–30% | |
| Haematocrit (PCV) | Men | 40–54% |
| Women | 37–47% | |
Glossary of Terms Used
Emphysema:
It means stretching of body tissue due to the accumulation of gas or air in the tissue or organ. Pulmonary emphysema is a chronic lung disease in which air sacs of the lungs are stretched until the elastic fibers in them are destroyed.
Polycythemia:
It is an excess of red blood cells. It may be temporary due to lack of oxygen in the blood. It may be due to heart disease or continued exposure to high altitudes. Also, if may be due to disorder of the bone marrow.
Myeloid leukemia:
It is a kind of blood cancer.
Congenital heart disease:
It means any heart disorder that is present at birth. Most common is a hole between two ventricles, either narrowing or the wrong position of the aorta (the main artery), or constriction of valves on the left side of the heart with weakness of the heart muscle.
Aplastic anemia:
It is a disease of the bone marrow. It produces deficiency of the red blood cells, white blood cells as well as platelets.
Infectious mononucleosis:
Also called glandular fever caused by a herpes virus (Ebstein–Barr virus).
Megaloblastic anemia:
It is a disease of the bone marrow. Here, immature abnormal red blood cells are found in the blood.
Edema:
Swelling of any part of the body due to retention of fluids.
Sub–acute bacterial endocarditis:
Endocarditis means inflammation of the endocardium, the inner lining of the heart. When bacteria infects it, then it is called bacterial endocarditis. All types of endocarditis, if untreated are fatal.
Microcytic anemia:
A decrease in red blood cells, reduced hemoglobin, PCV, MCV, MCH and MCHC.
Macrocytic anemia:
A decrease in red blood cells, reduced, hemoglobin, elevated MCH and MCV with normal MCHC.
Physical & Chemical Examination
A sufficient quantity of the morning specimen (5–6ml) is collected in a dry container and given to a pathological lab for examination.
Physical Examination
| A. |
Consistency: Normal consistency – well formed.
A sufficient quantity of the morning specimen (5–6ml) is collected in a dry container and given to a pathological lab for examination.
|
||||||||||||||||
| B. |
Color: Normal color – light to dark brown (due to the presence of bile pigments)
|
||||||||||||||||
| C. |
Presence of adult worms or their parts like
|
||||||||||||||||

Chemical Examination
Normal stools are slightly acidic, slightly alkaline or neutral. The pH values range from 5.8 to 7.5.
| 1. | Strongly acidic stool (pH below 5.5) indicates an excess of carbohydrates in the diet. It is non–pathologic. But, if fermentation is present, it may be due to lactose intolerance. Then, it is pathologic. | |
| 2. | Strongly alkaline stool (pH above 7.5) indicates an excess of protein in the diet. It is non–pathologic. | |
| 3. | Occult blood: Generally it is not present. If there, it indicates either infection or some disorder of the digestive system. | |
| 4. | Reducing substances: They are generally found in stools of infants suffering from diarrhea |
Microscopic Examination of Feces
Cells
| 1. | Pus Cells: Normally, a few are present. More than a few indicates bacillary dysentery or ulcerative colitis. | |
| 2. | Epithelial Cells: Normally a few are present. If many are present, however, it indicates inflammation of the bowels. | |
| 3. | Macrophages: Normally, present only occasionally. If many are present, it indicates bacillary dysentery or ulcerative colitis. | |
| 4. | Erythrocytes (Red Blood Cells): Normally absent. If present, it indicates lesions in the colon, rectum or the anus. If clumped, it means amoebiasis (a kind of infective dysentery). |
Crystals
| 1. | Triple phosphate or calcium oxalate crystals: Normally present due to indigestion of foods like spinach, tomatoes, berries etc. | |
| 2. | Charcot Leyden crystals: Normally absent. If present, it indicates ulcerative conditions or amoebiasis | |
| 3. | Hematoidin crystals: Normally absent. If present, it indicates intestinal hemorrhage. |
Vegetable Matter
| 1. | Normally present as residual constituents. |
Animal Matter
| 1. | Normally present as residual contents, or undigested fibers. |
Undigested Ingredients
| 1. | Starch: Normally absent. If present in a high proportions, it indicates indigestion. | |
| 2. | Fat: Normally absent. If present in high proportions, it indicates indigestion. |
Other Findings
| 1. | Yeast cells: Normally present. | |
| 2. | Bacteria: Normally gram negative are present. |
If a high percentage of gram positive bacteria are present, it indicates intestinal ulceration.
Intestinal Protozoa
There are pathogenic and non–pathogenic protozoa found in stool.
| A. | Non–pathogenic
|
|||||||||||||
| B. | Pathogenic
|
Nematohelminths
They are pathogenic in nature. The different kinds of worms found are:
| 1. | Enterobius vermicularis (pinworm). | |
| 2. | Trichuris trichuria (whipworm).
|
|
| 3. | Ascaris lumbricoides (roundworm).
|
|
| 4. | Ankylostoma duodenale (hookworm). | |
| 5. | Nectar americanus. | |
| 6. | Strongyloides stercoralis. |
Platyhelminths
They are pathogenic in nature:
| 1. | Taenia saginata. | |
| 2. | Taenia solium (tape worms). |
The different kinds of tape worms found are:
| 1. | Beef tape worm. | |
| 2. | Pork tape worm. | |
| 3. | Dwarf tape worm. | |
| 4. | Dog tape worm. |
Trematodes
They are pathogenic in nature, generally known as fluke:
| 1. | Schistosoma hematobium. | |
| 2. | Schistosoma mansoni.
|
|
| 3. | Schistosoma japonicum. |
Special Blood Tests
Determination of Erythrocyte Sedimentation Rate (ESR)
When anti–coagulated blood is allowed to stand undisturbed for some time, the red blood cells start to settle down. The rate at which red blood cells settle down is known as the Erythrocyte sedimentation rate.
It is done by three methods:
| 1. | Westergren’s method. | |
| 2. | Wintrobe’s method. | |
| 3. | Micro–sedimentation (Landau) method. |
Normal Range
| Method | Male | Female |
| Westergren’s method | 0–15 mm. after 1st hour | 0–20 mm. after 1 hour |
| Wintrobe’s method | 0–9 mm.after 1st hour | 0–20 mm. after 1 hour |
| Landau method | 0–5 mm after 1st hour | 0–8 mm after 1 hour |
 |
ESR is increased in infections like tuberculosis, rheumatic fever, myeloma, Kala Azar, other chronic infections. | |
 |
ESR is greater in women than men due to difference in PCV (Packed Cell Volume). | |
 |
In certain anemias, ESR gradually increases after the third month and returns to normal after three to four weeks after delivery. | |
 |
ESR is low in infants and gradually increases as the child grows to puberty. | |
 |
The determination of ESR is useful in checking the progress of disease. The changes of ESR are not diagnostically of any specific disease. |
Determination of Platelet Count
To investigate bleeding disorders, determination of platelets is required.
Normal range: 2,50,000 – 5,00,000/cu mm (ml).
Many times prolonged bleeding and poor clot formation is due to Thrombocytopenia (decreased platelet count).
It is also found in aplastic anemia, megaloblastic anemia, hypersplenism and acute leukemia.
Thrombocytosis (increased platelet count) is found in polycythemia vera, following splenectomy and in chronic myelogenous leukemia.
Splenectomy – is the surgical removal of the spleen.
Hypersplenism – in this spleen is enlarged.
Meaning of other terms is given in routine blood tests.
Determination of Reticulocyte Count
It is done to determine red cell forming activity of the bone marrow.

 |
Normal Range: Adults – 0.2 to 2%. Infants – 2 to 6%. |
|
 |
Reticulocyte is a precursor of Red Blood Cells (RBCs). Reticulocyte count is reflection or erythropoetic activity (red blood cell forming activity) of the bone marrow. | |
 |
Increase in the number of reticulocyte indicates increased activity of the bone marrow, in hemolytic anemia or acute blood loss. It is known as reticulocytosis. | |
 |
Absence or low count of reticulocytes indicates bone marrow suppression in aplastic anemia. |
Determination of Absolute Eosinophil Count
 |
Normal Range: 40 to 440/cu mm (ml). | |
 |
Increased eosinophil count indicates certain leukemia, allergic reactions, parasitic infections and brucellosis. | |
 |
Decreased eosinophil count indicates Cushing’s Syndrome (increase in adrenal function). |
Brucellosis is an infectious disease mainly of cattle, dogs, pigs, goats, and occasionally, of humans. In humans, it is contracted by infected milk and is commonly known as undulant fever or malta fever.
Routine Coagulation Tests
When a blood vessel is damaged, bleeding stops by a process called hemostasis. First, the blood vessel contracts which reduces blood flow. Second, platelets form a plug, and third, clot formation occurs.
In blood coagulation, thrombin which is formed from prothrombin acts on soluble fibrinogen in the presence of Ca++ ions to form numerous insoluble fibrin threads. These threads criss–cross with one another. Erythrocytes (RBC) and Leucocytes (WBC) are entangled in their interstices and clots are formed.
The routine coagulation test is carried out for:
| 1. | Patients who have to undergo a major surgery. | |
| 2. | Patients who have a history of spontaneous bleeding after trauma or surgery |
The routine hemorrhagic disorder tests include:
| 1. | Bleeding time. | |
| 2. | Clotting time. | |
| 3. | Clot retraction and lysis time. | |
| 4. | Prothrombin time. | |
| 5. | Plasma recalcification time. | |
| 6. | Partial thromboplastin time. | |
| 7. | Activated partial thromboplastin time. | |
| 8. | Thrombin time. | |
| 9. | Fibrinogen determination. | |
| 10. | Protamine sulphate test. |
Normal Range
| Bleeding time | 1 – 5 minutes |
| Blood Clotting time | 4 – 5 minutes |
| Clot reaction & lysis time | Of 50% of clot retraction occurs at the end of 1 hr at 37 C, it is abnormal. Normal lysis time is 72 hrs. |
| Prothrombin Time | 14 (I) 2 seconds |
| Plasma recalcification time (RT) | Platelet rich plasma: 100 – 150 seconds Platelet poor plasma: 135 – 240 seconds |
| Partial thromboplastin time (PTT) | 60 to 80 seconds |
| Activated partial thromboplastin time (APTT) | 35 to 40 seconds |
| Thrombin Time | 15 to 20 seconds |
| Fibrinogen | 200 to 400 mg/dl |
| Protamine Sulphate test | if – to ++ is normal |
Special Hematological Tests
| 1. | Sickle Cell Anemia Screening. | |
| 2. | Determination of Fetal Hemoglobin. | |
| 3. | Determination of Osmotic Fragility of Red Blood Cells. | |
| 4. | Determination of Lupus Erythematosus (LE) Cell. | |
| 5. | Determination of Heinz Bodies. | |
| 6. | Determination of Blood Parasites. | |
| 7. | Determination of Glucose: 6 – Phosphate Dehydrogenase (46–PD). | |
| 8. | Determination of Iron and Total Iron Binding Capacity (TIBC) in Serum. | |
| 9. | Determination of Electrophoretic Fractionation of Hemoglobin. | |
| 10. | Microscopic Examination of Bone Marrow and Detection of Iron. | |
| 11. | Different tests to be performed in Different Bleeding Disorders. |
Sickle Cell Anemia Screening
| 1. | Normal blood does not have sickle cells. | |
| 2. | Clinical findings in S C Anemia. | |
| 3. | Normocytic, normochromic red cells. | |
| 4. | Presence of nucleated RBC, sickle cells and Howell–Jolly bodies. | |
| 5. | Increased reticulocytes. | |
| 6. | Increased platelets. | |
| 7. | Decrease in osmotic fragility of RBC. | |
| 8. | Hemoglobin electrophoresis shows particular hemoglobin. | |
| 9. | Positive sickle cell test. |
Determination of Fetal Hemoglobin
High level of fetal hemoglobin (HBF) is found in B–thalassemia major patient. Mild but significant rise is observed in (HBF) in B–thalassemia trait, sickle cell disease and in other congenital or acquired hematological conditions. Various percentage of HBF observed.
| Condition | HBF % |
| Normal | < 1% (Adults) |
| B – thalassemia major | 10–98% |
| Thalassemia | Reduced |
| Sickle cell trait | Normal |
| Sickle cell anemia | 1–20% |
Determination of Osmotic Fragility of Red Blood Cells
This is useful in determining hereditary spherocytosis, thalassemia and sick cell anemia. Here the Median Corpuscular Fragility (MCF) is determined.
| Condition | MCF |
| Normal | 0.45% or little lower. |
| Hereditary spherocytosis. | 0.5%. |
| Sickle Cell Anemia and Thalassemia. | 0.35% to 0.4%. |
Determination of Lupus Erythematosus (LE) Cell
Lupus Erythematosus is a disorder of collagen. Collagen is a fibrous, insoluble protein in connective tissue. If the test shows the presence of LE cells, it indicates the disorder.
Determination of Heinz Bodies
It is useful in detecting metabolic defects caused due to the deficiency of G–6 – PD or glutathione. The test is positive even when a patient is undergoing therapy with drugs such as anti–malarials and suphonamides.
Detection of Blood Parasites
Given in Routine Hematological (Blood) Tests.
Determination of Glucose: 6 – Phosphate Dehydrogenase (G6 – PD)
Glucose – 6 – phosphate dehydrogenase deficiency is hereditary disorder. Presence of this enzyme is required in red blood cells to protect hemoglobin from oxidation. Absence of this enzyme is harmless unless red blood cells are exposed to antipyretics, anti–malarial drugs and sulphonamides.
| Observations | Decolorization time |
| Normal | 30 – 60 minutes. |
| 4 – 6 PD deficient | 140 minutes to 24 hours. |
| 4 – 6 carriers | 90 minutes to several hours. |
Determination of Iron and Total Iron Binding Capacity (TIBC) in Serum
Normal Values: Serum Iron: 60 – 150 mg/dl || Serum TIBC: 270 – 380 mg/dl
 |
Decrease in the serum iron level is due to chronic blood loss or nephrosis (any disorder of the kidney that is caused by any degenerative process other than infections). | |
 |
Increase in the serum iron level is due to hemolytic anemia, lead poisoning, pyridoxine deficiency, pernicious anemia and necrotic hepatitis (Necrosis means death of a small area of tissue within an organ). | |
 |
Decrease in serum TIBC is found in cirrhosis (a type of permanent and progressive liver damage), hemochromatosis and nephrosis. | |
 |
Increase in serum TIBC is found in different states of chronic iron deficiency and nephrosis. |
Determination of Electrophoretic Fractionation of Hemoglobin
Hemoglobin is a conjugated protein when it is subjected to an electrical field, the different proteins depending upon their speeds towards the anode (at pH 8.9). Normal and abnormal hemoglobin have different velocities. This helps in identifying congenital disorders of hemoglobin.
Microscopic Examination of Bone Marrow and Detection of Iron
This test is conducted in various anemias like aplastic, megaloblastic, sideroblastic. It is also done in acute leukemias, multiple myeloma (malignant tumor of the bone marrow) and diseases of the reticuloendothelial system (network of very thin tissue that lines the lymphatic and blood vessels, the heart and various other body cavities). In iron deficiency anemias, iron is very low but in sideroblastic anemia it is increased.
Different Tests to be Performed in Different Bleeding Disorders
| Bleeding Disorder | Laboratory Test |
| Vascular defect platelet defect. | Bleeding time. |
| Coagulation factor deficiency. | Clotting time. Plasma recalcification time. Activated partial thromboplastin time test (APTT). |
| Liver disorder and Vitamin K deficiency. | (Increased) APTT. (Increased) prothrombin time. |
| Hemophilia (Antihemophilic factor ‘A’ [AHF] deficiency). | Clotting time. APTT. |
| Excessive fibrinolysis. | Clot lysis test. Protamine sulphate test. |
| Christmas disease (Plasma thromboplastin component (PTC) or antihemophilic factor ‘B’ or Christmas factor. | Antihemophilic factor ‘B’ assay. |
| Von Willebrand’s disease (vWD). It is combination of vascular defect, platelet defect and antihemophilic factor ‘A’[AHF] deficiency. | (Abnormal)Bleeding time. (Abnormal) Clotting time. (Increased) APTT. (Platelet count normal). |
Determination of Possible Blood Group of A Child
| Blood Group | Father | Mother | Possible Group Of Child |
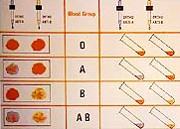
|
A | A | A |
| A | O | A or O | |
| AB | B | AB or A or B | |
| A | B | A or B or O or AB |
Indirect Antiglobulin (coomb’s) Test
This test is performed to detect presence of Rh antibodies or other antibodies in patient’s serum, in the following cases:
| 1. | To check whether an Rh negative woman (married to Rh positive husband) has developed anti Rh antibodies. | ||||||||||
| 2. | Anti D may be produced in the blood of any Rh negative person by exposure to D antigen by
|
Compatibility or Cross’ Matching Test
This is done before transfusion of blood to a patient of the cross–matching as non–compatible blood should never be transfused. Minor cross match results are also important but in an emergency one can use blood with minor incompatibility.
Semi–quantitative determination of Anti–D Antibody Titer
This is useful to defect hemolytic disease of the newborn.
Tests to be Performed and Criteria for Blood Transfusion
Most important tests performed are:
| 1. | Blood grouping and Rh factor. | |
| 2. | Antibody detection by indirect antiglobulin (Coomb’s) test for a typical, incomplete antibodies. |
Other tests performed on collected blood are
| 1. | Hepatitis – B surface antigen. | |
| 2. | AIDS antibodies. | |
| 3. | Syphilis (VDRL) test. | |
| 4. | Malarial parasites. |
Criteria accepted for selection of donor
 |
The age should be above 18 – 60 years. | |
 |
Hemoglobin should not be less than 12.5 g/dl. | |
 |
Interval of 16 weeks should be there between two donations. | |
 |
Pulse rate should be regular and between to 78 – 100/min. | |
 |
Accepted Blood Pressure. Systolic: between 90 – 150 mm Hg. Diastolic: between 50 – 100 mm Hg. |
|
 |
Body temperature of donor should be normal. | |
 |
Absence of any chronic disease. |
The donor is rejected if
| 1. | There is a history of viral hepatitis or AIDS. | |
| 2. | There is a history of malaria for the last three years. | |
| 3. | If the patient has received immunization against rabies, mumps, rubella, small pox within two months. | |
| 4. | If the donor has undergone dental surgery within 72 hours. |
Glucose Tolerance Test (GTT)
Glucose tolerance means the ability of the body to utilize glucose in blood circulation. Glucose tolerance is reduced in diabetes mellitus and in certain endocrine gland (Endocrine Gland: a ductless body organ which produces hormones that affect and help control various other organs. There are several such glands – thyroid, parathyroid, ovaries, testes, adrenals, pineal, pituitary and pancreas islet cells) disorders like hyperthyroidism, hyperpituitarism and hyperadrenalism. Blood sugar in the case of a normal person remains fairly constant throughout the day. There is temporary rise in blood sugar levels after food which depends upon the type of food consumed. This increase remains up to two to three hours and then returns to normal. Diminished glucose tolerance is observed when the ability of the body to utilize glucose decreases. The rise in blood sugar or glucose is greater than in a normal person. Also, a return of blood glucose levels to the normal fasting level is slow.
This is observed in Type 1.
| 1. | Diabetes mellitus. | |
| 2. | Hyperactivity of thyroid, pituitary and adrenals. | |
| 3. | Injection of cortisone like hormone. | |
| 4. | Increased secretion of the growth hormone. | |
| 5. | Very severe liver disease. | |
| 6. | Glycogen storage disease of the liver due to the limited capacity of a person to store excess glycogen. | |
| 7. | Severe infection of staphylococcal bacilli or even common cold. |
| Time | Fasting | 1/2 hour | 1 hour | 1 1/2 hours | 2 hours | 2 1/2 hours |
| After taking glucose | ||||||
| 3 Blood Glucose gm/dl | 70 | 130 | 145 | 105 | 75 | 80 |
| Urine Glucose – Absent throughout the test | ||||||
| Normal renal threshold for glucose = 150 – 170 mg/dl. | ||||||
Raised renal threshold after ingestion of glucose up to 250 – 300 mg/dl occurs with increasing age and prolonged diabetes mellitus. Lowered renal threshold (130 – 150 gm/dl) is observed in abnormality of tubular re–absorption of glucose. Extended glucose tolerance curve (instead of two and a half hours goes up to four to five hours) is observed in insulin secreting tumors of the pancreas. It is also observed in Simmond’s disease which causes hypoglycemia (means reduction of sugar or glucose levels. It drops to below 60 mg/dl and affects brain cells).
Determination of Glycosylated Hemoglobin
The red blood cells of a normal person and children above six months old contain three genetically determined hemoglobin species HbA – 90%, HbA2 – 2.5% and HbF – 0.5% of total hemoglobin content of RBC. Besides these hemoglobins, other variants of hemoglobin present are HbAla – 1.6%, HbAlb – 0.8% and HbAlc – 4%. They are products of non–enzymatic, post–synthetic transformation of HbA. Their rate of formation depends upon the lifespan of RBCs and its mean hexose concentration. These are collectively measured as HbA – abc or HbAl. HbAl indicates the average blood sugar concentration for an extended time period. It remains unaffected by the short term fluctuations in blood sugar levels. HbAl levels term fluctuations in blood sugar level. HbAl levels reflect carbohydrate imbalance better than fasting glucose concentration or the GTT (Glucose Tolerance Test). The determination of HbAl is a convenient and suitable test as it helps evaluate the adequacy of diabetic control in the prevention of various diabetic complications.
Normal Range: 4 – 7%.
Regulation of Sugar and Types of Diabetes
Concentration of blood sugar (glucose) remains steady up to 100 mg/dl during 24 hours. After partaking of food, it increases up to 140 – 150 mg/dl.
The ways by which glucose is added to the blood:
| 1. | Absorption from the intestine. | |
| 2. | By the breakdown of liver glycogen (glycogen is a starch like carbohydrate) to glucose. | |
| 3. | By gluconeogenesis (a form of glucose from non–carbohydrates). |
The ways by which glucose is removed from the blood:
| 1. | By synthesis of fats e.g. triglycerides. | |
| 2. | Conversion to liver glycogen. | |
| 3. | Conversion to muscle glycogen. | |
| 4. | In synthesis of glycoproteins and lactose etc. |
When these processes are performed in the right balance, the blood sugar level remains within the normal limits of about 70 – 110 mg/dl. throughout the day. (Average 100 mg/dl).
 |
The liver plays an important part by taking glucose from the blood and converting it into glycogen. | |
 |
Releasing glucose from glycogen and converting pyruvate to glucose. | |
 |
Muscle glycogen does not contribute directly to blood sugar. Glycogenolysis in the muscle produces locate, which is converted into glucose in the liver. | |
 |
Kidney plays its part by the re–absorption of glucose when the blood glucose level is below 150 – 170 mg/dl (threshold level). |
In normal individuals, the blood glucose level does not rise above the threshold level.
The following hormones play a part:
| A. |
Insulin: It is secreted by the pancreas. It controls blood sugar in the following ways:
Glucose is also regulated by other hormones than insulin but to a lesser extent. These hormones antagonize the action of insulin. They are: |
|||||||||||||||||||
| B. | Thyroxine (secreted by the thyroid gland). | |||||||||||||||||||
| C. | Glucagon (secreted by alpha cells of the pancreas). | |||||||||||||||||||
| D. | Growth hormone (secreted by the pituitary gland). | |||||||||||||||||||
| E. | Glucocorticoids (secreted by the adrenal cortex). | |||||||||||||||||||
| F. | Epinephrine (secreted by the adrenal medulla). |
These hormones increase blood sugar levels by:
| 1. | By increasing absorption of glucose from the intestine. | |
| 2. | Decreasing the oxidation of glucose or glycogen to pyruvate and lactate. | |
| 3. | Preventing synthesis of glycogen. | |
| 4. | Stimulating synthesis of glycogen from glucose. | |
| 5. | Stimulating the formation of glucose from non–carbohydrates. |
Glucose travels throughout body and when it comes in contact with beta cells of pancreas, they secrete insulin in response to increased levels of glucose in the blood. This insulin attaches itself to each cell surface to make glucose molecules enter the cells to be used for energy. The cells require very little energy and the rest is stored as adenosine triphosphate (ATP). This is then used by the body. Everything in excess is stored by the muscles, the liver etc. In case of a normal person, the fasting blood sugar level is 70 – 110 mg/dl. It does not fall below 70 mg/dl due to the antagonizing effect of other hormones mentioned above. When the blood sugar rises to a relatively high level, the kidney filters it through glomeruli (network of tiny blood vessels) but it returns to the blood by the re–absorption system of its tubules.
Diabetes Mellitus
Diabetes Mellitus occurs when blood glucose is too high due to very less insulin or none at all. Sometimes, the pancreas produces normal amounts of insulin but the body needs more than the normal. As a result of this, the body suffers from a lack of energy. People with diabetes often complain of weakness and tiredness.
Characteristics of diabetes mellitus
 |
Raised fasting blood sugar levels. | |
 |
The amount of urine passed is increased often up to 5 to 6 liters of pale urine. | |
 |
Thirst. | |
 |
Due to lack of insulin glucose is not utilized by cells. Energy is obtained through Body proteins and Fats. This causes muscular weakness and results in weight loss. Also, the end product of protein is urea which increases above the normal range and causes discomfort. |
|
 |
In severe cases, more fat is used for energy. The excessive oxidation of fatty acids increases ketone bodies in the blood and there is also an increase in cholesterol synthesis. | |
 |
In severe cases, the plasma bicarbonate decreases which results in a fall of blood pH and leads to a loss of sodium ions. |
The last two conditions may result in diabetic coma.
Types of Diabetes
There are two major types of diabetes. Type I and Type II
| A. | Type I Diabetes:
It is insulin dependent diabetes mellitus (IDDM) or “Juvenile diabetes.” This occurs when beta cells of the pancreas do not function to produce insulin. Patients take supplementary insulin by injections because if taken orally it will get digested, as insulin is a protein in nature. Insulin is either obtained from the pancreas of cattle or pigs, or produced synthetically, using recombinant DNA (deoxyribonucleic acid). This synthetic insulin does not stimulate the formation of antibodies against insulin as the animal insulin may do. Most often young people get this type of diabetes and the onset is fast. Sometimes, older people also get Type I diabetes which has a slow onset and acts like Type II for a long period. |
|
| B. | Type II Diabetes:
This is non–insulin dependent diabetes mellitus (NIDDM). The body produces some insulin but the requirement is more. It may be due to reduction in the number of insulin producing beta cells. Due to this, glucose is unable to enter the cells as interaction between insulin and its receptor is less effective. People with this type of diabetes are usually above their ideal weight. Overeating also contributes to it, so diet is primary treatment for this type of diabetes. Generally people above the age of 40 get this type of diabetes, but it may be found in younger people also. About 85% of all people who have diabetes, have Type II diabetes. |
Other Types of Diabetes
Some people are not diabetic but may have an increased risk of developing diabetes.
 |
Pre–diabetes: A person both of whose parents are diabetic, or who has an identical twin who develops diabetes, although he/she may not have diabetes initially is considered a prospect for the disease. | |
 |
Latent diabetes: Some people have elevated blood glucose levels only in certain times of stress e.g. in pregnancy or during severe infection. They suffer from diabetes but become normal when pregnancy ends or after they recover from the infection. |
Tabular Representation of the Special Blood Tests
| Test | Normal Values | |
| Creatine Phospokinase | Male | 16 – 110 U/L |
| Female | 16 – 94 U/L | |
| Creatine Kinase (MB) | Normally, CK–MB activity is less than 5 U/lt. And accounts for less than 3 per cent of the total CPK activity. Myocardial infarction is suggested by CK – MB > 5% of Total CK Activity. | |
| Lactate Dehydrogenase | 160 – 319 U/lt. (At 30° C) | |
| Serum Amylase | Up to 95 U/lt | |
| Serum Lipase | 20 – 300 U/lt. (At 30° C) | |
| Fasting Blood Sugar | 80 – 120 mgs/dl | |
| Post Prandial Blood Sugar | up to 160 mgs/dl | |
| Glycosylated Hemoglobin | < 7% | Normal |
| 7 – 8% | Excellent Control | |
| 8 – 9% | Good Control | |
| 9 – 10% | Fair Control | |
| > 10% | Poor Control | |
| Serum Cerruloplasmin | 0.20 – 0.55 gms/lt | |
| Serum Iron | 40 – 130 micrograms/dl | |
| Serum Iron Binding Capacity | 210 – 385 micrograms/dl | |
| Plasma Fibrinogen | 200 – 400 mgs/dl | |
| Serum Ferritin | Male | 20 – 400 ng/ml |
| Female | 10 – 130 ng/ml | |
| Serum Ammonia | Normal: 11–35 Umol/lt | |
| Serum Uric Acid | 2 – 7 mgs/dl | |
| Serum Acid Phosphatase | Up to 12 U/lt | |
| Leptospira IgM | < 10 | Negative |
| 10 – 20 | Low Positive | |
| > 20 | Positive | |
| Tuberculosis IgG | Less than 225 Units/ml | |
| Tuberculosis IgA | Less than 350 Units/ml | |
| Fructosamine | Normal Range | 1.6 – 2.6 m mol/l |
| Satisfactory Control | 2.6 – 3.2 m mol/l | |
| Mediocre Control | 3.6 – 3.7 m mol/l | |
| Poor Control | 3.7 – 4.5 m mol/l | |
| Carcinoembryonic Antigen (CEA) | Smokers | Not detectable to 5.2 ng/ml |
| Non–smokers | Not detectable to 3.4 ng/ml | |
| Alpha Feto Protein | 0 – 20 IU/ml | |
| In Pregnancy | ||
| Maternal Serum | Gestational Age | |
| 15 weeks | 8.9 – 61.1 | |
| 16 weeks | 10.2 – 56.2 | |
| 17 weeks | 15.6 – 59.3 | |
| 18 weeks | 16.5 – 79.3 | |
| 19 weeks | 18.9 – 86.1 | |
| 20 weeks | 18.5 – 103.9 | |
Diabetic Profile Tests
These can be categorized into three groups of tests
| A. | Group I Tests: These tests when performed give us an idea of the severity of diabetes mellitus.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| B. | Group II Tests: These tests when performed gives us an idea of the disturbed lipid (fat) metabolism and atheroma (it is an abnormal condition where walls of arteries are clogged with fatty tissue). Serum (fasting) sample is required of these tests.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
| C. | Group III Tests: These tests are performed in acidosis (a serious condition in which the body’s acid – alkali balance is disturbed) and ketosis (in this, excessive amounts of ketones are formed when fat is used instead of sugar to provide energy (Ketone is a substance which results during the breakdown of fats and fatty acids into carbon dioxide and water). These tests are done to know the acid-base balance of the body.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
Renal Profile Tests
Normal Values
| Test | Normal Values |
| Blood Urea | 15 – 50 mgs/dl |
| Blood Urea Nitrogen | 5 – 20 mgs/dl |
| Serum Creatinine | 0.4 – 1.2 mgs/dl |
| Serum Calcium | 8.8 – 11 mgs/dl |
| Serum Phosphorous | 2.0 – 5.0 mgs/dl |
| Serum Magnesium | 1.5 – 2.5 mgs/dl |
| Serum Sodium | 134 – 146 m Eq/lt |
| Serum Potassium | 3.4 – 4.8 m Eq/lt |
| Serum Chlorides | 96 – 106 m Eq/lt |
| Serum Bicarbonate | 22 – 26 m Eq/lt |
Liver Function Tests – Normal Values
| Test | Normal Values |
| Serum Bilirubin | Less than 1 mgs/dl |
| SGOT (AST) | Upto 40 units /lt |
| SGPT (ALT) | Upto 40 units/lt |
| GGPT | Male: 8 – 38 units/lt |
| Serum Alkaline Phosphates | Adults: 26 – 99 mu/ml |
Lipid Profile – Normal Values
| Test | Normal Values | |
| Serum Cholesterol | American Heart Association recommendation | Normal up to 200 mgs/dl |
| Borderline | Upto 239 mgs/dl | |
| Elevated if > 240 mgs/dl. on repeated values. | ||
| Serum Triglycerides | < 180 mgs/dl. normal. Values vary depending on diet, alcohol, metabolic state, exercise etc. Elevation of values to be considered only if repeated values are high. | |
| HDL Cholesterol | 30 – 60 mgs/dl | |
| LDL Cholesterol | 100 – 190 mgs/dl | Borderline |
| >190 mgs/dl. | Risk | |
| Formula for calculating LDL Cholesterol is INVALID if TGL > 400 mgs/dl. | ||
| Total/HDL Ratio | < 4 | Normal |
| 4 – 6 | Low Risk | |
| > 6 | High Risk | |
Hormonal Assays
Normal Values
| Test | Normal Values | |
| Free T4 | 0.8 – 2.0 ng/dl | |
| Free T3 | 2.3 – 4.2 pg/ml | |
| TSH* | 0.25 – 4.30 microunits/ml | |
| Serum T3* | 70 – 200 ng/dl | |
| Serum T4* | 4.0 – 11.0 micrograms/dl | |
| Follicle Stimulating Hormone* | Male | Not detectable to 20 miu/ml |
| Female | ||
| Follicular Phase | 5 – 20 miu/ml | |
| Midcycle Peak | 15 – 35 miu/ml | |
| Luteal Peak | 5 – 20 miu/ml | |
| Post–Menopausal | 40 – 200 miu/ml | |
| Luteinising Hormone* | Male | Not detectable to 25 miu/ml |
| Female | ||
| Post–Menopausal | 5 – 20 miu/ml | |
| Ovulating Females | ||
| Follicular Phase | Upto 8 miu/ml | |
| Mid–cycle Peak | 7 – 50 miu/ml | |
| Luteal Phase | Upto 7 miu/ml | |
| Prolactin | Male | Not detectable to 15 ng/ml |
| Female | Not detectable to 20 ng/ml | |
| In Pregnancy | ||
| I Trimester | 7 – 31 ng/ml | |
| II Trimester | 31 – 182 ng/ml | |
| III Trimester | 84 – 232 ng/ml | |
| One day Post–partum | 20 – 319 ng/ml | |
| Testosterone | Male | 300 – 1,300 ng/dl |
| Female | 30 – 95 ng/dl | |
| Free Testosterone | Male | 9 – 30 ng/dl |
| Female | 0.3 – 1.9 ng/dl | |
| 17 – Ketosteroids | Male | 9 – 24 mgs/day |
| Female | 5 – 17 mgs/day | |
| 17 – Ketogenic Steroids | Male | 8 – 26 mgs/day |
| Female | 6 – 18 mgs/day | |
| Serum Calcitonin | 0.02 – 0.04 ng/ml | |
| Serum Cortisol | A.M. 4.3 – 22.6 microgram/dl | |
| P.M. 3.10 – 16.6 microgram/dl | ||
| Parathormone | Not detectable to 27 ng/dl | |
| DHEA Sulphates | Male | 80 – 560 microgram/dl |
| Female | 35 – 430 microgram/dl | |
| Beta HCG | Less than 10 | |
| I Month | 20 – 1,000 | |
| I Trimester | 10,000 – 1,60,000 | |
| II Trimester | 6,000 – 30,000 | |
Tests done on Automated Chemiluminescent System.
Routine Urine Examination
Physical Examination of Urine

Routine urine examination is detailed analysis of urine. It helps detect alterations in the composition of the urine which help in the diagnosis of many disorders. When a sample of urine is submitted to a pathological laboratory, the following examinations are done:
Physical Examination
Volume:
 |
Normal volume of an early morning mid–stream sample is 50 – 300ml. | |
 |
If it is more than 500ml, it indicates diabetes or polyuria (frequent passing of urine). | |
 |
If it is less than 20ml, it indicates some kidney disorder. |
Color:
 |
The normal color of urine is pale yellow. | |
 |
If it is dark yellow to orange, it indicates some liver disorder. | |
 |
If it is white, it shows the presence of pus. | |
 |
If it is pink to red, it indicates the presence of red blood cells. | |
 |
If it is brownish black, it indicates the presence of melanin or homogenistic acid (a rare disorder). | |
 |
If it is blue to green, it is a liver disorder. |
Sometimes, due to the intake of some food or medicines also, one could notice a change in the color or their urine e.g. the intake of beet imparts a reddish color to urine. The intake of vitamin B capsules gives a dark yellow color to it, if rimfamycin is taken, it gives an orange tinge to the urine.
Appearance:
 |
Usually, it is clear, sometimes, it is cloudy. | |
 |
Sometimes, it is turbid due to the presence of WBCs (White Blood Cells), epithelial cells. | |
 |
Sometimes, it is hazy due to mucus. | |
 |
Smoky, due to red blood cells. | |
 |
Milky due to chyle (lymph). |
Reaction:
 |
Usually acidic pH range 4.5 – 7.5. | |
 |
If pH less than 4.7 it is more acidic. | |
 |
If pH more than 7.5 it is more alkaline. |
Odor:
 |
Usually, it is aromatic in normal conditions. | |
 |
It has a fruity odor in diabetes. | |
 |
Ammoniacal odor in cases of urine retention. | |
 |
Foul smelling due to urinary tract infection. |
Sediment formation at the bottom of a container after collection:
 |
Usually, there is no or very little formation of sediment in normal conditions. | |
 |
If pus cells, red blood cells, cysts or epithelial cells are present, the sedimentation rate ranges from moderate to high. |
Specific Gravity:
 |
Usually varies from 1.003 to 1.060. | |
 |
A low special gravity indicates diabetes insipidus or kidney infection (chronic). | |
 |
High specific gravity indicates diabetes mellitus or acute kidney infection. |
Chemical Examination of Urine
Protein:
 |
Normally absent. | |
 |
Present in kidney disorders, dehydration, heart disease, and severe diarrhea. Sometimes, due to an excessive muscular exercise, prolonged cold baths, excessive protein intake or vaginal discharge in the urine, the test shows the presence of protein. |
Glucose:

 |
Normally absent. | |
 |
If present, it indicates diabetes mellitus or hyperactivity of the endocrine glands. | |
 |
It can be present after brain injury or coronary thrombosis. |
Ketone bodies:
 |
Normally absent. | |
 |
If test shows ketones, it is due to severe diabetes mellitus, fevers, certain nervous disorders or prolonged diarrhea and vomiting. | |
 |
Even when a person starves, the urine shows a presence of ketone bodies. |
Bile pigments:
 |
Normally absent. | |
 |
Present in liver disorders. |
Bile salts:
 |
Normally absent. | |
 |
Present in liver disorders. |
Urobilinogen:
 |
Normally present in very low concentrations. | |
 |
Increased in liver disorders. |
Blood:
 |
Normally absent. | |
 |
Present in acute kidney infections, kidney cancer, tuberculosis of the kidneys, chronic infections, stone formation in the kidneys, severe burns or a reaction to blood transfusion. |
Additional Chemical Tests
Non–glucose Sugars:
 |
Lactose: May be present normally. It is present in lactating women. | |
 |
Fructose: Present in liver disorders. | |
 |
Pentoses: Are present due to drug therapy or hereditary conditions. |
Non–glucose reducing substances:
 |
Ascorbic acid: Present in Vitamin C therapy. | |
 |
Salicylic acid: Due to drugs having salicilates. | |
 |
Menthol: Due to the intake of food containing menthol. |
Nitrite:
 |
Present due to bacterial infection |
Indican:
 |
It is present in very low concentrations. | |
 |
It is increased due to intestinal obstruction, cholera, typhoid fever or peritonitis. | |
 |
Sometimes, it is due to the intake of diets rich in proteins. |
Microscopic Examination of Urine
Pus Cells:
 |
Normally 2 to 3 pus cells are present in HPF (high power field of microscope). | |
 |
If more than 5 it indicates urinary tract infection or non infectious condition such as fever, stress, dehydration irritation to urethra, bladder or urethra. |
Epithelial cells:
 |
Normally two to three present in males. | |
 |
Normally two to five present in females. | |
 |
More than five epithelial cells per HPF indicates tubular damage, pyelonephritis or kidney transplant rejection. |
Casts:

 |
Normally absent. | |
 |
There are hyaline cysts, red cell cysts, white cell cysts, granular cysts, waxy cysts, and fatty cysts. They are present due to kidney disorders. | |
 |
Occasional Hyaline cysts may be present due to physical exercise and physiological dehydration. | |
 |
Granular cysts may be present after strenuous exercise for a short duration. |
Amorphous Material:
 |
Amorphous urates of sodium, potassium or calcium are present normally. | |
 |
Amorphous phosphates of calcium and magnesium are present normally. |

Crystals:
 |
Uric acid, calcium sulphate, calcium oxalate and ammonium magnesium phosphate (triple phosphate) crystals are indicative of the presence of kidney stones. | |
 |
Hippuric acid, calcium carbonate, ammonium biurate and calcium phosphate crystals are non–significant. | |
 |
Following crystals, found in acidic urine indicate abnormal metabolism – cystine, cholesterol, leucine, tyrosine, bilirubin, hematoidin and sulphonamides. |
Bacteria:
 |
Normally absent. | |
 |
If present indicates infection. |
Yeast cells:
 |
Normally absent. | |
 |
May be present in acidic urine containing sugar. |
Parasites:
 |
Normally absent. | |
 |
If present, they are Trichomonas Vaginalis (from vagina) or Trichononas Hominis (from rectum). |
Diabetes inspidus:
It is disorder due to hormonal imbalance. Kidneys become overactive and a person urinates excessively. A person has a raging thirst and an increased appetite.
Diabetes mellitus:
It is a disorder in which the body cannot make use of sugars and starches in a normal way.
Peritonitis:
It is inflammation of the peritoneum – the membrane that lines the abdominal cavity and covers the abdominal organs.
Pyelonephritis:
It is an inflammation of the kidney and the renal pelvis (the hollow cone into which urine flows from the kidney).
Endocrine glands:
It is a ductless body organ which produces hormones. These hormones affect and help control various other organs.
Occult blood:
“Occult” means hidden. Here blood is present in very minute traces. It is not visible to the naked eyes.











