Toll Free No.: 1800 2330 0007 email: admin@dhanwantari.com

Nervous System
NEUROPHYSIOLOGY
Neurophysiology has been a subject of study since as early as 4,000 B.C. Neurophysiology is connected with electrophysiology, neurobiology, psychology, neurology, clinical neurophysiology, neuroanatomy, cognitive science, biophysics, mathematical biology, and other brain sciences.
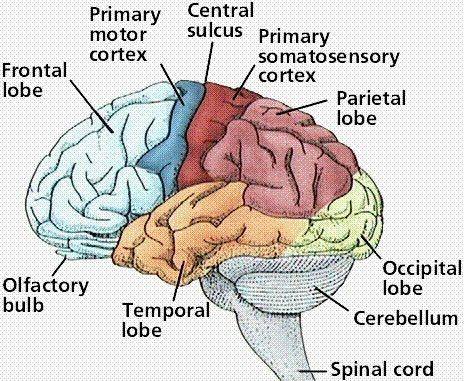
Brain
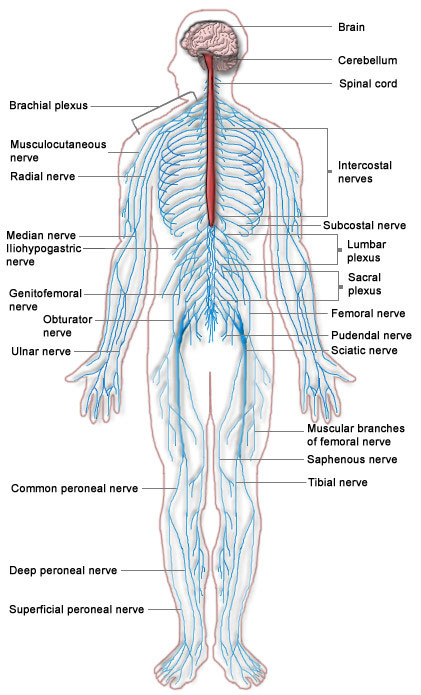
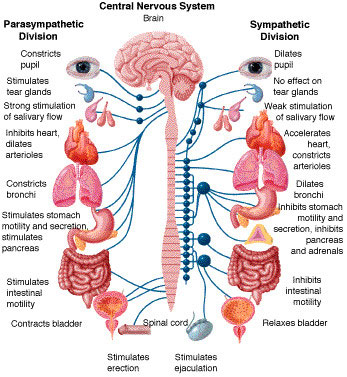
The nervous system consists of cells that communicate information about an organism's surroundings and itself. The nervous system of humans is divided into the central nervous system (CNS) and peripheral nervous system (PNS).
The brain is the center of the nervous system in all vertebrate and most invertebrate animals.
The brain can be subdivided into several distinct regions:
| 1. | The Cerebral Hemispheres: Form the largest part of the brain, occupying the anterior and middle cranial fossae in the skull and extending backwards over the tentorium cerebelli. They are made up of the cerebral cortex, the basal ganglia, tracts of synaptic connections, and the ventricles containing CSF. | |
| 2. | The Diencephalon: (Not shown above) includes the thalamus, hyopthalamus, epithalamus and subthalamus, and forms the central core of the brain. It is surrounded by the cerebral hemispheres. | |
| 3. | The Midbrain: (Not shown) is located at the junction of the middle and posterior cranial fossae. | |
| 4. | The Pons: Sits in the anterior part of the posterior cranial fossa- the fibres within the structure connect one cerebral hemisphere with its opposite cerebellar hemisphere. | |
| 5. | The Medulla Oblongata: Is continuous with the spinal cord, and is responsible for automatic control of the respiratory and cardiovascular systems. | |
| 6. | The Cerebellum: Overlies the pons and medulla, extending beneath the tentorium cerebelli and occupying most of the posterior cranial fossa. It is mainly concerned with motor functions that regulate muscle tone, coordination, and posture. |
The cerebral hemispheres can be further divided into four lobes:
| 1. | The frontal lobe is concerned with higher intellectual functions, such as abstract thought and reason, speech (Broca's area in the left hemisphere only), olfaction, and emotion. Voluntary movement is controlled in the precentral gyrus (the primary motor area). | |
| 2. | The parietal lobe is dedicated to sensory awareness, particularly in the postcentral gyrus (the primary sensory area). It is also concernes with abstract reasoning, language interpretation and formation of a mental egocentric map of the surrounding area. | |
| 3. | The occipital lobe is responsible for interpretation and processing of visual stimuli from the optic nerves, and association of these stimuli with other nervous imputs and memories. | |
| 4. | The temporal lobe is concerned with emotional development and formation, and also contains the auditory area responsible for processing and discrimination of sound. It is also the area thought to be responsible for the formation and processing of memories. |
Arousal
Perhaps the most obvious aspect of the behavior of any animal is the daily cycle between sleeping and waking. Arousal and alertness also controlled by an extensive network of brain areas.
Homeostasis
For any animal, survival requires maintaining a variety of parameters of bodily state within a limited range of variation: these include temperature, water content, salt concentration in the bloodstream, blood glucose levels, blood oxygen level, and others
Motivation
According to evolutionary theory, all species are genetically programmed to act as though they have a goal of surviving and propagating offspring. At the level of an individual animal, this overarching goal of genetic fitness translates into a set of specific survival-promoting behaviors, such as seeking food, water, shelter, and a mate.[105] The motivational system in the brain monitors the current state of satisfaction of these goals, and activates behaviors to meet any needs that arise. The motivational system works largely by a reward–punishment mechanism. When a particular behavior is followed by favorable consequences, the reward mechanism in the brain is activated, which induces structural changes inside the brain that cause the same behavior to be repeated later, whenever a similar situation arises. Conversely, when a behavior is followed by unfavorable consequences, the brain's punishment mechanism is activated, inducing structural changes that cause the behavior to be suppressed when similar situations arise in the future.
Learning and Memory
Working Memory: Is the ability of the brain to maintain a temporary representation of information about the task that an animal is currently engaged in
Episodic Memory: Is the ability to remember the details of specific events. This sort of memory can last for a lifetime
Semantic Memory: Is the ability to learn facts and relationships
Instrumental learning: Is the ability for rewards and punishments to modify behavior.
Motor Learning: Is the ability to refine patterns of body movement by practicing, or more generally by repetition.
In vertebrates, the nervous system can be split into two parts, the central nervous system (brain and spinal cord), and the peripheral nervous system.
The human brain alone contains around one hundred billion neurons and one hundred trillion synapses; it consists of thousands of distinguishable substructures, connected to each other in synaptic networks.
Translational research and medicine
Neurology, psychiatry, neurosurgery, psychosurgery, anesthesiology, neuropathology, neuroradiology, clinical neurophysiology and addiction medicine are medical specialties that specifically address the diseases of the nervous system. These terms also refer to clinical disciplines involving diagnosis and treatment of these diseases. Neurology works with diseases of the central and peripheral nervous systems, such as amyotrophic lateral sclerosis (ALS) and stroke, and their medical treatment. Psychiatry focuses on affective, behavioral, cognitive, and perceptual disorders. Anesthesiology focuses on perception of pain, and pharmacologic alteration of consciousness. Neuropathology focuses upon the classification and underlying pathogenic mechanisms of central and peripheral nervous system and muscle diseases Neurosurgery and psychosurgery work primarily with surgical treatment of diseases of the central and peripheral nervous systems.
What are some disorders of the nervous system?
The nervous system is vulnerable to various disorders. It can be damaged by the following:
| 1. | trauma | |
| 2. | infections | |
| 3. | degeneration | |
| 4. | structural defects | |
| 5. | tumors | |
| 6. | blood flow disruption | |
| 7. | autoimmune disorders |
Disorders of the nervous system
Disorders of the nervous system may involve the following:
| 1. | vascular disorders - such as stroke, transient ischemic attack (TIA), subarachnoid hemorrhage, subdural hemorrhage and hematoma, and extradural hemorrhage | |
| 2. | infections - such as meningitis, encephalitis, polio, and epidural abscess | |
| 3. | structural disorders - such as brain or spinal cord injury, Bell's palsy, cervical spondylosis, carpal tunnel syndrome, brain or spinal cord tumors, peripheral neuropathy, and Guillain-Barré syndrome | |
| 4. | functional disorders - such as headache, epilepsy, dizziness, and neuralgia | |
| 5. | degeneration - such as Parkinson's disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS), Huntington's chorea, and Alzheimer's disease |
Signs and symptoms of nervous system disorders
The following are the most common general signs and symptoms of a nervous system disorder. However, each individual may experience symptoms differently. Symptoms may include:
| 1. | persistent or sudden onset of a headache | |
| 2. | a headache that changes or is different | |
| 3. | loss of feeling or tingling | |
| 4. | weakness or loss of muscle strength | |
| 5. | sudden loss of sight or double vision | |
| 6. | memory loss | |
| 7. | impaired mental ability | |
| 8. | impaired mental ability | |
| 9. | lack of coordination | |
| 10. | muscle rigidity | |
| 11. | tremors and seizures | |
| 12. | back pain which radiates to the feet, toes, or other parts of the body | |
| 13. | muscle wasting and slurred speech |
The symptoms of a nervous system disorder may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
Physicians who treat nervous system disorders
Physicians who treat nervous system disorders may have to spend a lot of time working with the patient before making a probable diagnosis of the specific condition. Many times, this involves performing numerous tests to eliminate other conditions, so that the probable diagnosis can be made.
| Neurology | Neurological Surgery | Rehabilitation for Neurological Disorders |
| The branch of medicine that manages nervous system disorders is called neurology. The medical doctors who treat nervous system disorders are called neurologists. | The branch of medicine that provides surgical intervention for nervous system disorders is called neurosurgery, or neurological surgery. Surgeons who operate as a treatment team for nervous system disorders are called neurological surgeons or neurosurgeons. | The branch of medicine that provides rehabilitative care for patients with nervous system disorders is called physical medicine and rehabilitation. Physicians who work with patients in the rehabilitation process are called physiatrists. |
Diagnostic Tests for Neurological Disorders

What are some diagnostic tests for nervous system disorders?
Evaluating and diagnosing damage to the nervous system is complicated and complex. Many of the same symptoms occur in different combinations among the different disorders. To further complicate the diagnostic process, many disorders do not have definitive causes, markers, or tests.
In addition to a complete medical history and physical examination, diagnostic procedures for nervous system disorders may include the following:
| 1. | Computed tomography scan (also called a CT or CAT scan) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce both horizontal and vertical cross-sectional images (often called slices), of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
| 2. | Electroencephalogram (EEG) - a procedure that records the brain's continuous electrical activity by means of electrodes attached to the scalp. | |
| 3. | Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. | |
| 4. | Electrodiagnostic tests [i.e., electromyography (EMG) and nerve conduction velocity (NCV)] - studies that evaluate and diagnose disorders of the muscles and motor neurons. Electrodes are inserted into the muscle, or placed on the skin overlying a muscle or muscle group, and electrical activity and muscle response are recorded. | |
| 5. | Positron emission tomography (PET) - in nuclear medicine, a procedure that measures the metabolic activity of cells. | |
| 6. | Arteriogram (also called an angiogram) - an x-ray of the arteries and veins to detect blockage or narrowing of the vessels. | |
| 7. | Spinal tap (also called a lumbar puncture) - a special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. | |
| 8. | Evoked potentials - procedures that record the brain's electrical response to visual, auditory, and sensory stimuli. | |
| 9. | Myelogram - a procedure that uses dye injected into the spinal canal to make the structure clearly visible on x-rays. | |
| 10. | Neurosonography - a procedure that uses ultra high-frequency sound waves that enable the physician to analyze blood flow in cases of possible stroke. | |
| 11. | Ultrasound (also called sonography) - a diagnostic imaging technique which uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. Ultrasounds are used to view internal organs as they function, and to assess blood flow through various vessels. |
What is neurological surgery?
Neurological surgery, also called neurosurgery, is the branch of medicine that provides both operative and nonoperative management of disorders that affect the central and peripheral nervous systems, including their supportive structures and vascular supply, and the operative and non-operative management of pain.
Neurological surgery encompasses disorders of the brain, spine, and nerves, including the following:
| 1. | The extracranial and intracranial carotid and vertebral arteries | |
| 2. | Disorders of the pituitary gland | |
| 3. | Tumors in and around the brain | |
| 4. | Disorders of the spinal cord, meninges, and spine, including those which may require treatment by removing or replacing intervertebral discs, spinal fusion, or instrumentation | |
| 5. | Disorders of the peripheral nerves | |
| 6. | Disorders of the autonomic nervous system |
The surgeon who specializes in neurological surgery is called a neurosurgeon or neurological surgeon.
Acute Spinal Cord Injury
What is an acute spinal cord injury?
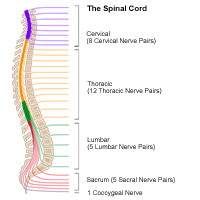
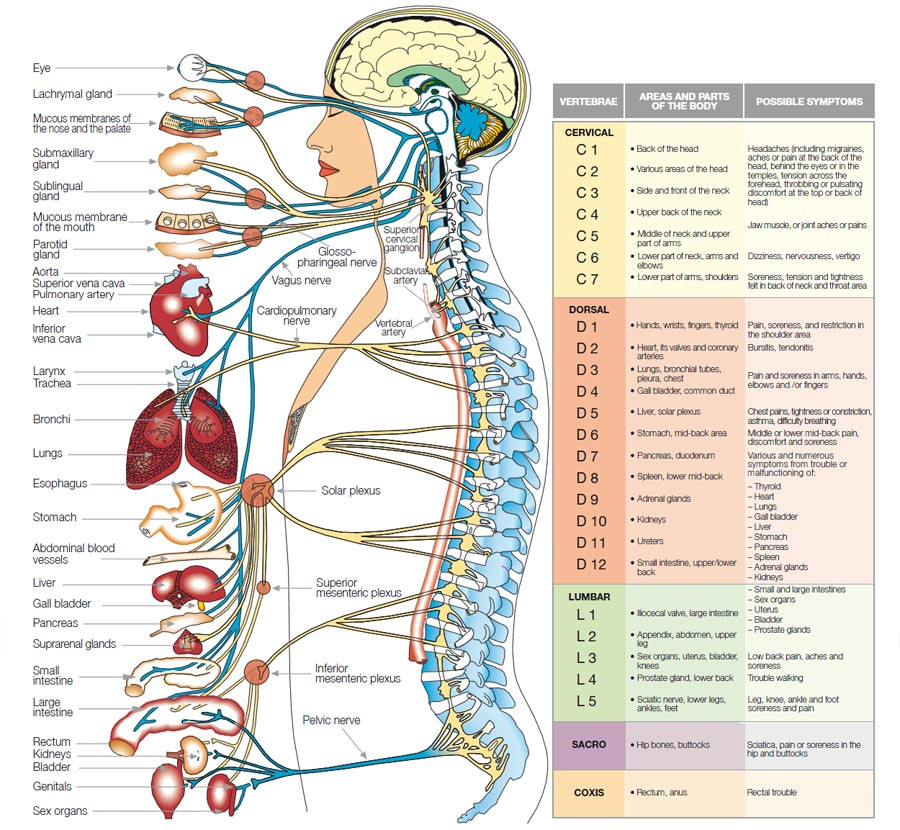
The spinal cord is a bundle of nerves that carries messages between the brain and the rest of the body.
Acute spinal cord injury (SCI) is due to a traumatic injury that either results in a bruise (also called a contusion), a partial tear, or a complete tear (called a transection) in the spinal cord. SCI is a common cause of permanent disability and death in children and adults.
About 12,000 people a year sustain a spinal cord injury. As many as 231,000 to 311,000 people in the US are living with a spinal cord injury, according to the Spinal Cord Injury Information Network. More than half of all SCIs occur among young people between the ages of 16 and 30 years. The majority of SCI victims (80.9 percent) are male.
What causes an acute spinal cord injury?
There are many causes of SCI. The more common injuries occur when the area of the spine or neck is bent or compressed, as in the following:
| 1. | Birth injuries, which typically affect the spinal cord in the neck area | |
| 2. | Falls | |
| 3. | Motor vehicle accidents (automobiles, motorcycles, and being struck as a pedestrian) | |
| 4. | Sports injuries | |
| 5. | Diving accidents | |
| 6. | Trampoline accidents | |
| 7. | Violence (gun shot or stab wounds) | |
| 6. | Infections that form an abscess on the spinal cord |
What are the symptoms of an acute spinal cord injury?
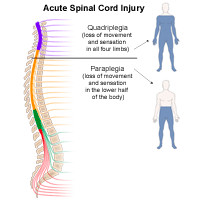
After a traumatic event, a person may have varying degrees of symptoms associated with the severity and location of the SCI. The location of the injury on the spinal cord will determine how severe the injury will be. For example, an injury that damages the cervical spine (in the neck area) can cause loss of muscle function or strength in all four extremities (arms and legs). This is referred to as tetraplegia (formerly called quadriplegia). An injury of this type often requires mechanical breathing assistance, as with a ventilator, as the chest muscles may also be weakened. An injury to a lower part of the spinal cord that causes paralysis and loss of function in the legs and lower body is called paraplegia.
The extent of the damage to the spinal cord determines whether the injury is complete or incomplete. A complete injury means that there is no movement or feeling below the level of the injury. An incomplete injury means that there is still some degree of feeling or movement below the level of the injury.
Initially after a spinal cord injury, the patient may experience spinal shock, which causes loss or decrease in feeling, muscle movement, and reflexes. As swelling subsides, other symptoms may appear depending on the location of the injury. Generally, the higher up the level of the injury is to the spinal cord, the more severe the symptoms. For example, an injury to the neck, at C1 or C2 (the first and second vertebrae in the spinal column), and especially in the mid-cervical vertebrae of C3, C4, and C5, affects the respiratory muscles and the ability to breathe. A lower injury, in the lumbar vertebrae, may affect nerve and muscle control to the bladder, bowel, and legs.
The following are the most common symptoms of acute spinal cord injuries. However, each individual may experience symptoms differently. Symptoms may include:
| 1. | Muscle weakness | |
| 2. | Loss of voluntary muscle movement in the chest, arms, or legs | |
| 3. | Breathing problems | |
| 4. | Loss of feeling in the chest, arms, or legs | |
| 5. | Loss of bowel and bladder function |
The symptoms of SCI may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
How are acute spinal cord injuries diagnosed?
The full extent of the SCI may not be completely understood immediately after the injury, but may be revealed with a comprehensive medical evaluation and diagnostic testing. Acute SCI is a medical emergency. Anytime there is a suspicion of injury to the spinal cord, emergent medical attention is absolutely necessary. The diagnosis of SCI is made with a physical examination and diagnostic tests. During the examination, the physician obtains a complete medical history and inquires as to how the injury occurred. Trauma to the spinal cord can cause neurological problems and requires further medical follow-up. Occasionally, surgery is necessary to stabilize the spinal cord after acute SCI.
Diagnostic tests may include:
| 1. | Blood tests | |
| 2. | X-ray - a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film | |
| 3. | Computed tomography scan (also called a CT or CAT scan) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body; A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
| 4. | Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body |
Treatment of an acute spinal cord injury
Specific treatment for an acute spinal cord injury will be determined by your physician based on:
| 1. | Your age, overall health, and medical history | |
| 2. | Extent of the SCI | |
| 3. | Type of SCI | |
| 4. | Your tolerance for specific medications, procedures, or therapies | |
| 5. | Expectations for the course of the SCI | |
| 6. | Your opinion or preference |
SCI requires emergency medical attention on the scene of the accident or injury. This is accomplished by immobilizing the head and neck areas to prevent the patient from moving. This may be very difficult since the victim and/or bystanders may be very frightened after the traumatic incident. There is currently no way to repair a damaged or bruised spinal cord, though researchers are actively seeking means of stimulating spinal cord regeneration. The severity of the SCI and the location determines if the SCI is mild, severe, or fatal. Surgery is sometimes necessary to evaluate the injured cord, stabilize fractured back bones, decompress (or release) the pressure from the injured area, and to manage any other injuries that may have been a result of the accident. Treatment is individualized, depending on the extent of the condition and the presence of other injuries.
Treatment may include:
| 1. | Observation and medical management in the intensive care unit (ICU) | |
| 2. | Medications, such as corticosteroids (to help decrease the swelling in the spinal cord) | |
| 3. | Mechanical ventilator, a breathing machine (to help the patient breathe) | |
| 4. | Bladder catheter - a tube that is placed into the bladder that helps to drain the urine into a collection bag | |
| 5. | Feeding tube (placed through the nostril to the stomach, or directly through the abdomen into the stomach, to provide extra nutrition and calories) |
Recovery from a SCI requires long-term hospitalization and rehabilitation. An interdisciplinary team of physicians, nurses, therapists (physical, occupational, or speech), and other specialists work to medically manage the patient to control pain, to monitor the heart function, blood pressure, body temperature, nutritional status, bladder and bowel function, and attempt to control involuntary muscle shaking (spasticity). Rehabilitation focuses on preventing muscle wasting and contractures, and works to retrain the patient to use other muscles to aid in mobility and movement. Some of the important chronic complications of SCI include pressure ulcers (so-called "bed sores") and pneumonia.
Life-long considerations for a person with a SCI
A traumatic event that results in a SCI is devastating to the person and the family. The healthcare team educates the family after hospitalization and rehabilitation on how to best care for the person at home and outlines specific clinical problems that require immediate medical attention by the patient's physician. The disabled person requires a focus on maximizing his or her capabilities at home and in the community. Positive reinforcement will encourage him or her to strengthen his or her self-esteem and promote independence. A person with a SCI requires frequent medical evaluations and diagnostic testing following hospitalization and rehabilitation to monitor his or her progress.
Alzheimer's Disease
What is Alzheimer's disease?
Alzheimer's disease is a progressive, neurodegenerative disease that occurs when nerve cells in the brain die and often results in the following:
| 1. | Impaired memory, thinking, and behavior | |
| 2. | Confusion | |
| 3. | Restlessness | |
| 4. | Personality and behavior changes | |
| 5. | Impaired judgment | |
| 6. | Impaired communication | |
| 7. | Inability to follow directions | |
| 8. | Language deterioration | |
| 9. | Impaired thought processes that involve visual and spatial awareness | |
| 10. | Emotional apathy |
With Alzheimer's disease, motor function is often preserved.
When Alzheimer's was first identified by German physician, Alois Alzheimer, in 1906, it was considered a rare disorder. Today Alzheimer's disease is recognized as the most common cause of dementia (a disorder in which mental functions deteriorate and break down). An estimated 5.3 million Americans have Alzheimer's disease. According to the Alzheimer's Association, this number includes 5.1 million people over the age of 65, as well as 200,000 to 500,000 people younger than 65 who have early-onset Alzheimer's and other types of dementias.
How is Alzheimer's different from other forms of dementia?
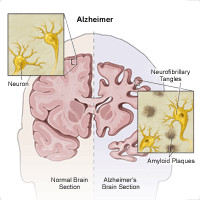
Alzheimer's disease is distinguished from other forms of dementia by characteristic changes in the brain that are visible only upon microscopic examination during autopsy. Brains affected by Alzheimer's disease often show presence of the following:
| 1. | Fiber tangles within nerve cells (neurofibrillary tangles) | |
| 2. | Clusters of degenerating nerve endings (neuritic plaques) |
Another characteristic of Alzheimer's disease is the reduced production of certain brain chemicals necessary for communication between nerve cells, especially acetylcholine, as well as norepinephrine, serotonin, and somatostatin.
What causes Alzheimer's disease?
Although intense investigation has been underway for many years, the causes of Alzheimer's disease are not entirely known. Suspected causes often include the following:
| 1. | Age and family history. | |
| 2. | Certain genes. | |
| 3. | Abnormal protein deposits in the brain. | |
| 4. | Other risk and environmental factors | |
| 5. | Immune system problems |
What are the warning signs or symptoms of Alzheimer's disease?
According to the Alzheimer's Association, the following are the most common symptoms of Alzheimer's disease. However, each individual may experience symptoms differently. Symptoms may include:
| 1. | Memory loss that affects job skills, especially short-term memory loss | |
| 2. | Difficulty performing familiar tasks | |
| 3. | Problems with language | |
| 4. | Disorientation to time and place | |
| 5. | Poor or decreased judgment | |
| 6. | Problems with abstract thinking | |
| 7. | Misplacing things | |
| 8. | Changes in mood or behavior | |
| 9. | Changes in personality | |
| 10. | Loss of initiative | |
| 11. | Loss of ability to recognize who people are, even people well known to the individual, such as his or her child or spouse, when the disease progresses to a severe stage |
The symptoms of Alzheimer's disease may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
How is Alzheimer's diagnosed?
There is not a single, comprehensive test for diagnosing Alzheimer's disease. By ruling out other conditions through a process of elimination, physicians, or other specialists, can obtain a diagnosis of probable Alzheimer's disease with approximately 90 percent accuracy. However, the only way to confirm a diagnosis of Alzheimer's disease is through autopsy.
Examination and evaluation are essential in determining whether the dementia is the result of a treatable illness. In addition to a complete medical history and extensive neurological motor and sensory exam, diagnostic procedures for Alzheimer's disease may include the following:
| 1. | Mental status test - this is a brief and simple test of memory and some other common cognitive or thinking skills; it is usually part of a complete neurological exam | |
| 2. | Neuropsychological testing | |
| 3. | Blood tests | |
| 4. | Lumbar puncture (spinal tap) - a procedure performed by inserting a hollow needle into the lower back (lumbar spine) | |
| 5. | Urinalysis - laboratory examination of urine for various cells and chemicals, such as red blood cells, white blood cells, infection, or excessive protein | |
| 6. | Chest x-ray - a diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film | |
| 7. | Electroencephalogram (EEG) - a procedure that records the brain's continuous electrical activity by means of electrodes attached to the scalp | |
| 8. | Computed tomography scan (also called a CT or CAT scan) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
| 9. | Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body | |
| 10. | Genetic testing - some genetic testing is available, especially in some research settings; Because there is no cure or effective treatment for Alzheimer's, the decision to undergo genetic testing is one that requires careful consideration and counseling with a specialist in genetics. |
Prevention of Alzheimer's
Because the cause of the disease is unknown, there are no prevention protocols to follow at this time. And, because the controllable risk factors for Alzheimer's disease are unknown, it is not yet possible to reduce the chances of developing the disease.
Treatment for Alzheimer's
Specific treatment for Alzheimer's disease will be determined by your physician based on:
| 1. | Your age, overall health, and medical history | |
| 2. | Extent of the disease | |
| 3. | Your tolerance for specific medications, procedures, or therapies | |
| 4. | Expectations for the course of the disease | |
| 5. | Your opinion or preference |
At this time, there is no cure for Alzheimer's, no way of slowing down the progression of this disease, and no treatment available to reverse the deterioration of Alzheimer's disease. New research findings give reason for hope, and several drugs are being studied in clinical trials to determine if they can slow the progress of the disease or improve memory for a period of time.
There are some medications available to assist in managing some of the most troubling symptoms of Alzheimer's disease, including the following:
| 1. | Depression | |
| 2. | Behavioral disturbance | |
| 3. | Sleeplessness |
In managing the disease, physical exercise and social activity are important, as are proper nutrition, health maintenance, and a calm and well-structured environment.
Alzheimer's rehabilitation
The rehabilitation program for persons with Alzheimer's differs depending upon the symptoms, expression, and progression of the disease, and the fact that making a diagnosis of Alzheimer's is so difficult. These variables determine the amount and type of assistance needed for the Alzheimer's individual and family.
With Alzheimer's rehabilitation, it is important to remember that, although any skills lost will not be regained, the caregiving team must keep in mind the following considerations:
| 1. | In managing the disease, physical exercise and social activity are important, as are proper nutrition and health maintenance. | |
| 2. | Plan daily activities that help to provide structure, meaning, and accomplishment for the individual. | |
| 3. | As functions are lost, adapt activities and routines to allow the individual to participate as much as possible. | |
| 4. | Keep activities familiar and satisfying. | |
| 5. | Allow the individual to complete as many things by himself/herself as possible. The caregiver may need to initiate an activity, but allow the individual to complete it as much as he/she can. | |
| 6. | Provide "cues" for desired behavior (i.e., label drawers/cabinets/closets according to their contents). | |
| 7. | Keep the individual out of harm's way by removing all safety risks (i.e., car keys, matches). | |
| 8. | As a caregiver (full-time or part-time), it is important to understand your own physical and emotional limitations. |
Amyotrophic Lateral Sclerosis (ALS)
What is Amyotrophic Lateral Sclerosis (ALS)?
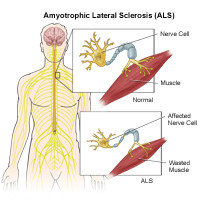
Amyotrophic lateral sclerosis (ALS) is a terminal neurological disorder characterized by progressive degeneration of nerve cells in the spinal cord and brain. Often referred to as "Lou Gehrig's disease" (a famous baseball player who died from the disease), it is one of the most devastating of the disorders that affects the function of nerves and muscles. ALS does not affect mental functioning or the senses (such as seeing or hearing), and it is not contagious. Currently, there is no cure for amyotrophic lateral sclerosis.
Statistics of ALS
Consider the following statistics regarding ALS:
| 1. | Most people who develop ALS are between the ages of 40 and 70, although the disease can occur at a younger age. | |
| 2. | ALS occurs throughout the world with no racial, ethnic, or socioeconomic boundaries. | |
| 3. | ALS affects as many as 30,000 Americans, with 5,600 new cases diagnosed in the US each year. |
What are the different types of ALS?
There are three known classifications of ALS, including the following:
| 1. | Sporadic: The most common form of ALS in the US, involving 90 percent to 95 percent of all cases. These cases occur randomly, without any known cause, and there is no association with persons in the family with the disease. | |
| 2. | Familial: Suggests that the disease is inherited and accounts for a very small number of cases in the United States, about 5 percent to 10 percent. | |
| 3. | Guamanian: An extremely high incidence of ALS was observed in Guam and the Trust Territories of the Pacific in the 1950's. |
What are the symptoms of ALS?
Patients who suffer from ALS initially experience weakness in one of their limbs that develops over a matter of days or, more commonly, a few weeks. Then, several weeks to months later, weakness develops in another limb. Sometimes the initial problem can be one of slurred speech or difficulty swallowing. As ALS progresses, though, more and more symptoms are noticed. The following are the most common symptoms of ALS. However, each individual may experience symptoms differently. Symptoms may include:
| 1. | Twitching and cramping of muscles, especially those in the hands and feet | |
| 2. | Loss of motor control in the hands and arms | |
| 3. | Impairment in the use of the arms and legs | |
| 4. | Tripping and falling | |
| 5. | Dropping things | |
| 6. | Persistent fatigue | |
| 7. | Uncontrollable periods of laughing or crying | |
| 8. | Slurred or thick speech and difficulty in projecting the voice |
As the disease progresses, symptoms may include:
| 1. | Difficulty breathing | |
| 2. | Difficulty swallowing | |
| 3. | Paralysis |
The symptoms of ALS may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is ALS Diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for ALS may include the following:
| 1. | Difficulty breathing | |
| 2. | Difficulty swallowing | |
| 3. | Paralysis |
The symptoms of ALS may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is ALS Diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for ALS may include the following:
| 1. | Laboratory tests (including blood and urine studies and thyroid functioning tests) | |
| 2. | Muscle and/or nerve biopsy - a procedure performed to remove tissue or cells from the body for examination under a microscope. | |
| 3. | Spinal tap (also called a lumbar puncture) - a special needle is placed into the lower back, into the spinal canal; This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. | |
| 4. | X-ray - a diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film | |
| 5. | Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body | |
| 6. | Electrodiagnostic tests (i.e., electromyography (EMG) and nerve conduction study, or NCS) - studies that evaluate and diagnose disorders of the muscles and motor neurons; Electrodes are inserted into the muscle, or placed on the skin overlying a muscle or muscle group, and electrical activity and muscle response are recorded. |
Treatment for ALS
Specific treatment for ALS will be determined by your physician based on:
| 1. | Your age, overall health, and medical history | |
| 2. | Extent of the disease | |
| 3. | Your tolerance for specific medications, procedures, or therapies | |
| 4. | Expectations for the course of the disease | |
| 5. | Your opinion or preference |
For most people with ALS, primary treatment may involve the management of symptoms, and may include physical, occupational, speech, respiratory, and nutritional therapies. Some medications and/or heat or whirlpool therapy may help to relieve muscle cramping. Exercise, although recommended in moderation, may help to maintain muscle strength and function.
There is no proven treatment for ALS. However, the US Food and Drug Administration (FDA) approved Rilutek®, the first drug that has prolonged the survival of persons with ALS.
Managing the symptoms of ALS is a process that may be challenging for people with the condition, their caregivers, and the medical team. However, it is important to know that there are many community resources available for support and assistance.
Researchers are conducting studies to increase their understanding of genes that may cause the disease, mechanisms that can trigger motor neurons to degenerate in ALS, and approaches to stop the progress leading to cell death.
Bell's Palsy
What is Bell's Palsy?
Bell's palsy is an unexplained episode of facial muscle weakness or paralysis that begins suddenly and worsens over three to five days. This condition results from damage to the 7th (facial) cranial nerve, and pain and discomfort usually occurs on one side of the face or head. It can strike anyone at any age, but it occurs most often in pregnant women, and people who have diabetes, influenza, a cold or another upper respiratory ailment. This nerve disorder affects about 40,000 US adults and children each year. Bell's palsy strikes men and woman equally. It is less common before age 15 or after age 60. Bell's palsy is not considered permanent, but in rare cases it does not disappear. Currently, there is no known cure for Bell's palsy; however, recovery usually begins two weeks to six months from the onset of the symptoms. The majority of people with Bell's palsy recover full facial strength and expression.
What causes Bell's palsy?
A specific cause of Bell's palsy is unknown, however, it has been suggested that the disorder is due to inflammation that is directed by the body's immune system against the nerve controlling movement of the face. The weakness or symptoms seen in Bell's palsy is sometimes seen in association with the following:
| 1. | Diabetes | |
| 2. | High blood pressure | |
| 3. | Trauma | |
| 4. | Toxins | |
| 5. | Lyme disease | |
| 6. | Guillain-Barré syndrome | |
| 7. | Sarcoidosis | |
| 8. | Myasthenia Gravis | |
| 9. | Infection, especially following a viral infection with Herpes simplex virus (a virus that is related to the cause of the common "cold sores" of the mouth) |
These conditions cause weakness through a different mechanism than the usual inflammation of Bell's palsy.
What are the Symptoms of Bell's Palsy?
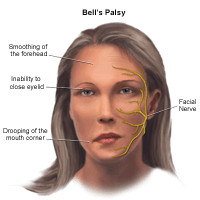
The following are the most common symptoms of Bell's palsy. However, each individual may experience symptoms differently. Symptoms may include:
| 1. | Disordered movement of the muscles that control facial expressions such as smiling, squinting, blinking, or closing the eyelid | |
| 2. | Loss of feeling in the face | |
| 3. | Headache | |
| 4. | Tearing | |
| 5. | Drooling | |
| 6. | Loss of the sense of taste on the front two-thirds of the tongue | |
| 7. | Hypersensitivity to sound in the affected ear | |
| 8. | Inability to close the eye on the affected side of the face |
The symptoms of Bell's Palsy may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
Treatment for Bell's Palsy
One uniformly recommended treatment for Bell's palsy is protecting the eye from drying at nighttime or while working at a computer. Eye care, which may include eye drops during the day, ointment at bedtime, or a moisture chamber at night, helps to protect the cornea from scratching, which is crucial to the management of Bell's palsy.
Your physician will establish an appropriate treatment protocol for your condition based on the severity of your symptoms and your medical profile. Other treatment options include:
| 1. | Steroid medications - to reduce inflammation | |
| 2. | Antiviral medications - such as acyclovir | |
| 3. | Analgesics or moist heat - to relieve pain | |
| 4. | Physical therapy to stimulate the facial nerve |
Some individuals may choose to use alternative therapies in the treatment of Bell's palsy, but there is no proof these alternative therapies actually make an absolute difference in a person's recovery. Such treatment may include:
| 1. | Relaxation | |
| 2. | Acupuncture | |
| 3. | Electrical stimulation | |
| 4. | Biofeedback training | |
| 5. | Vitamin therapy, including B12, B6, and the mineral zinc |
Brain Tumors
What is a Brain Tumor?
A brain tumor is an abnormal growth of tissue in the brain. The tumor can either originate in the brain itself (primary brain tumor), or come from another part of the body and travel to the brain (metastastic or secondary brain tumor). Brain tumors may be classified as either benign (non-cancerous) or malignant (cancerous), depending on their behavior.
A benign tumor does not contain cancer cells and usually, once removed, does not recur. Most benign brain tumors have clear borders, meaning they do not invade surrounding tissue. These tumors can, however, cause symptoms similar to cancerous tumors because of their size and location in the brain.
Malignant brain tumors contain cancer cells. Malignant brain tumors are usually fast growing and invade surrounding tissue. Malignant brain tumors very rarely spread to other areas of the body, but may recur after treatment. Sometimes, brain tumors that are not cancer are called malignant because of their size and location, and the damage they can do to vital functions of the brain.
Metastatic brain tumors are tumors that begin to grow in another part of the body, then spread to the brain through the lymph system and bloodstream. Common types of cancer that can travel to the brain include lung cancer, breast cancer, nasopharygeal cancer, melanoma (a type of skin cancer), and colon cancer. These cancers are described and treated based on the specific type of cancer. For example, breast cancer that has spread to the brain is still called breast cancer.
Facts about Brain Tumors
Consider the following facts about brain tumors from the American Cancer Society:
| 1. | About 22,300 persons in the U.S. (adults and children) will be diagnosed with malignant tumors of the brain or spinal cord during 2011. | |
| 2. | About 13,100 people in the U.S. will die from brain tumors in 2011. |
What causes brain tumors?
The majority of brain tumors have abnormalities of genes involved in cell cycle control, causing uncontrolled cell growth. These abnormalities are caused by alterations directly in the genes, or by chromosome rearrangements which change the function of a gene.
Patients with certain genetic conditions (e.g., neurofibromatosis, von Hippel-Lindau disease, Li-Fraumeni syndrome, and retinoblastoma) also have an increased risk of developing tumors of the central nervous system. There have also been some reports of people in the same family developing brain tumors who do not have any of these genetic syndromes.
Workers in oil refining, rubber manufacturing, and chemists may have a higher incidence of certain types of tumors, although not all studies have found such links. Which, if any, chemical toxin is related to an increase in tumors is unknown at this time.
Patients who have received radiation therapy to the head as part of prior treatment for other malignancies are also at an increased risk for new brain tumors.
What are the symptoms of a Brain Tumor?
The following are the most common symptoms of a brain tumor. However, each person may experience symptoms differently. Symptoms vary depending on the size and location of tumor. Many symptoms are related to an increase in pressure in or around the brain. There is no spare space in the skull for anything except the delicate tissues of the brain and its fluid. Any tumor, extra tissue, or fluid can cause pressure on the brain and result in increased intracranial pressure (ICP), which may result from one or more of the ventricles that drain cerebral spinal fluid (CSF, the fluid that surrounds the brain and spinal cord) becoming blocked and causing the fluid to be trapped in the brain. This increased ICP may cause the following:
| 1. | Headache | |
| 2. | Vomiting (usually in the morning) | |
| 3. | Nausea | |
| 4. | Irritability | |
| 5. | Drowsiness | |
| 6. | Depression | |
| 7. | Decreased cardiac and respiratory function and, eventually, coma if not treated |
Symptoms of brain tumors in the cerebrum (large, outer part of the brain) may include:
| 1. | Symptoms caused by increased intracranial pressure (ICP) | |
| 2. | Seizures | |
| 3. | Visual changes | |
| 4. | Slurred speech | |
| 5. | Paralysis or weakness on half of the body or face | |
| 6. | Drowsiness and/or confusion | |
| 7. | Personality changes/impaired judgment | |
| 8. | Short-term memory loss | |
| 9. | Gait disturbances | |
| 10. | Communication problems |
Symptoms of brain tumors in the brainstem (base of brain) may include:
| 1. | Symptoms caused by increased intracranial pressure (ICP) | |
| 2. | Seizures | |
| 3. | Endocrine problems (diabetes and/or hormone regulation) | |
| 4. | Visual changes or double vision | |
| 5. | Headaches | |
| 6. | Paralysis of nerves/muscles of the face, or half of the body | |
| 7. | Respiratory changes | |
| 8. | Clumsy, uncoordinated walk | |
| 9. | Hearing loss | |
| 10. | Personality changes |
Symptoms of brain tumors in the cerebellum (back of brain) may include:
| 1. | Symptoms caused by increased intracranial pressure (ICP) | |
| 2. | Vomiting (usually occurs in the morning without nausea) | |
| 3. | Headache | |
| 4. | Uncoordinated muscle movements | |
| 5. | Problems walking |
The symptoms of a brain tumor may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is a brain tumor diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for brain tumors may include the following:
| 1. | Neurological examination - your physician tests reflexes, muscle strength, eye and mouth movement, coordination, and alertness. | |
| 2. | Computed tomography scan (Also called a CT or CAT scan.) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs, such as the brain. CT scans are more detailed than general x-rays. | |
| 3. | Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. MRI is very helpful for looking at the brain and spinal cord. | |
| 4. | X-ray - a diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. | |
| 5. | Arteriogram (Also called an angiogram.) - an x-ray of the arteries and veins to detect blockage or narrowing of the vessels. (This test is used les often than in the past, as special CT or MRI angiogram techniques can now be used to look at blood vessels in the brain.) | |
| 6. | Myelogram - a procedure that uses dye injected into the spinal canal to make the structure clearly visible on x-rays. | |
| 7. | Spinal tap (Also called a lumbar puncture.) - a special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. | |
| 8. | Positron emission tomography (PET) - a type of nuclear medicine procedure. This means that a tiny amount of a radioactive substance, called a radionuclide (radiopharmaceutical or radioactive tracer), is injected into a vein during the procedure to assist in the examination of the tissue under study. Specifically, PET studies evaluate the metabolism of a particular organ or tissue, so that information about the physiology (functionality) and anatomy (structure) of the organ or tissue is evaluated, as well as its biochemical properties. Thus, PET may detect biochemical changes in an organ or tissue that can identify the onset of a disease process before anatomical changes related to the disease can be seen with other imaging processes such as computed tomography (CT) or magnetic resonance imaging (MRI). | |
| 9. | Magnetic resonance spectroscopy (MRS) - a procedure that produces images depicting function rather than shape. The equipment requires a special, highly complex facility. | |
| 10. | Biopsy of tumor - a procedure in which a sample of tissue is removed (with a needle or during surgery) to be looked at under a microscope. |
Diagnosis of a brain tumor depends mostly on the types of cells involved and the tumor location.
What are the different types of Brain Tumors?
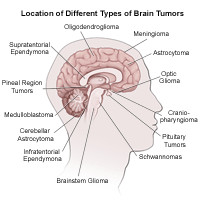
There are many different types of brain tumors. They are usually categorized by the type of cell where the tumor begins, or they are also categorized by the area of the brain where they occur. The most common types of brain tumors include the following:
A. Gliomas
The most common type of primary brain tumor is a glioma. Gliomas begin from glial cells, which are the supportive tissue of the brain. There are several types of gliomas, categorized by where they are found, and the type of cells that originated the tumor. The following are the different types of gliomas:
1. Astrocytomas: Astrocytomas are glial cell tumors that are derived from connective tissue cells called astrocytes. These cells can be found anywhere in the brain or spinal cord. Astrocytomas are the most common type of childhood brain tumor, and the most common type of primary brain tumor in adults. Astrocytomas are generally subdivided into high-grade, medium-grade or low-grade tumors. High-grade astrocytomas (glioblastomas) are the most malignant of all brain tumors. Astrocytomas are further classified for presenting signs, symptoms, treatment, and prognosis, based on the location of the tumor. The most common location of these tumors in children is in the cerebellum, where they are called cerebellar astrocytomas. These persons usually have symptoms of increased intracranial pressure, headache, and vomiting. There can also be problems with walking and coordination, as well as double vision. In adults, astrocytomas are more common in the cerebral hemispheres (cerebrum), where they commonly cause increased intracranial pressure (ICP), seizures, or changes in behavior.
2. Brain Stem Gliomas: Brain stem gliomas are tumors found in the brain stem. Most brain stem tumors cannot be surgically removed because of the remote location and delicate and complex function this area controls. Brain stem gliomas occur almost exclusively in children; the group most often affected is the school-age child. The child usually does not have increased intracranial pressure (ICP), but may have problems with double vision, movement of the face or one side of the body, or difficulty with walking and coordination.
3. Ependymomas: Ependymomas are also glial cell tumors. They usually develop in the lining of the ventricles or in the spinal cord. The most common place they are found in children is near the cerebellum. The tumor often blocks the flow of the CSF (cerebral spinal fluid, which bathes the brain and spinal cord), causing increased intracranial pressure. This type of tumor mostly occurs in children younger than 10 years of age. Ependymomas can be slow growing, compared to other brain tumors, but may recur after treatment is completed. Recurrence of ependymomas results in a more invasive tumor with more resistance to treatment. Two percent of brain tumors are ependymomas.
4. Optic Nerve Gliomas:Optic nerve gliomas are found in or around the nerves that send messages from the eyes to the brain. They are frequently found in children who have neurofibromatosis, a condition a child is born with that makes him/her more likely to develop tumors in the brain. Persons usually experience loss of vision, as well as hormone problems, since these tumors are usually located at the base of the brain where hormonal control is located. These are typically difficult to treat due to the surrounding sensitive brain structures.
5. Oligodendrogliomas: This type of tumor also arises from the supporting cells of the brain. They are found commonly in the cerebral hemispheres (cerebrum). Seizures are a very common symptom of these tumors, as well as headache, weakness, or changes in behavior or sleepiness. These tumors have a better prognosis than most other gliomas, but they can become more malignant with time. About two percent of brain tumors are oligodendrogliomas.
B. Metastatic Tumors
In adults, metastatic brain tumors are the most common type of brain tumors. These are tumors that begin to grow in another part of the body, then spread to the brain through the bloodstream. When the tumors spread to the brain, they commonly go to the part of the brain called the cerebral hemispheres, or to the cerebellum. Often, a patient may have multiple metastatic tumors in several different areas of the brain. Lung, breast, and colon cancers frequently travel to the brain, as do certain skin cancers. Metastatic brain tumors may be quite aggressive and may return even after surgery, radiation therapy, and chemotherapy.
C. Meningiomas
Meningiomas are usually benign tumors that come from the meninges, the tough outer coverings of the brain just under the skull. This type of tumor accounts for about one third of brain tumors in adults. They are slow growing and may exist for years before being detected. Meningiomas are most common in older patients, with the highest rate in people in their 70s and 80s. They are commonly found in the cerebral hemispheres just under the skull. They usually are separate from the brain and can sometimes be removed entirely during surgery. They can, however, recur after surgery and certain types can be malignant.
D. Schwannomas
Schwannomas are usually benign tumors, similar to meningiomas. They arise from the supporting cells of the nerves leaving the brain, and are most common on the nerves that control hearing and balance. When schwannomas involve these nerves, they are called vestibular schwannomas or acoustic neuromas. Commonly, they present with loss of hearing, and occasionally loss of balance, or problems with weakness on one side of the face. Surgery can be difficult because of the area of the brain in which they occur, and the vital structures around the tumor. Occasionally, radiation (or a combination of surgery and radiation) is used to treat these tumors.
E. Pituitary Tumors
The pituitary gland is a gland located at the base of the brain. It produces hormones that control many other glands in the body. These glands include the thyroid gland, the adrenal glands, the ovaries and testes, as well as milk production by pregnant women, and fluid balance by the kidney. Tumors that occur in or around the area of the pituitary gland can affect the functioning of the gland, or overproduce hormones that are sent to the other glands. This can lead to problems with thyroid functioning, impotence, milk production from the breasts, irregular menstrual periods, or problems regulating the fluid balance in the body. In addition, due to the closeness of the pituitary to the nerves to the eyes, patients may have decreased vision.
Tumors in the pituitary are frequently benign, and total removal makes the tumors less likely to recur. Since the pituitary is at the base of the skull, approaches for removal of a pituitary tumor may involve entry through the nose or the upper gum. Certain types of tumors may be treated with medication, which, in some cases, can shrink the tumor or stop the growth of the tumor.
F. Primitive Neuroectodermal Tumors (PNETs)
PNETs are much more common in children than in adults. They can occur anywhere in the brain, although the most common place is in the back of the brain near the cerebellum. When they occur here, they are called medulloblastomas. The symptoms depend on their location in the brain, but typically the patient experiences increased intracranial pressure. These tumors are fast growing and often malignant, with occasional spreading throughout the brain or spinal cord.
G. Medulloblastomas
Medulloblastomas are one type of PNET that are found near the midline of the cerebellum. This tumor is rapidly growing and often blocks drainage of the CSF (cerebral spinal fluid, which bathes the brain and spinal cord), causing symptoms associated with increased ICP. Medulloblastoma cells can spread (metastasize) to other areas of the central nervous system, especially around the spinal cord. A combination of surgery, radiation, and chemotherapy is usually necessary to control these tumors.
H. Craniopharyngiomas
Craniopharyngiomas are benign tumors that occur at the base of the brain near the nerves from the eyes to the brain, and the pituitary gland. These tumors are more common in children and comprise only about one percent of all brain tumors diagnosed in the U.S. Symptoms include headaches, as well as problems with vision. Hormonal imbalances are common, which may lead to poor growth in children. Symptoms of increased intracranial pressure may also be seen. Although these tumors are benign, they are hard to remove due to the sensitive brain structures that surround them.
I. Pineal Region Tumors
Many different tumors can arise near the pineal gland, a gland that helps control sleep and wake cycles. Gliomas are common in this region, as are pineal blastomas (a type of PNET). In addition, germ cell tumors, another form of malignant tumor, can be found in this area. Benign pineal gland cysts are also seen in this location, which makes the diagnosis difficult between what is malignant and what is benign. Biopsy or removal of the tumor is frequently necessary to tell the different types of tumors apart. Persons with tumors in this region frequently experience headaches or symptoms of increased intracranial pressure. Treatment depends on the tumor type and size.
What is the treatment for brain tumors?
Specific treatment for brain tumors will be determined by your physician based on:
| 1. | Your age, overall health, and medical history | |
| 2. | Type, location, and size of the tumor | |
| 3. | Extent of the condition | |
| 4. | Your tolerance for specific medications, procedures, or therapies | |
| 5. | Expectations for the course of the condition | |
| 6. | Your opinion or preference |
Treatment may include (alone or in combination):
| 1. | Surgery: Surgery is usually the first step in the treatment of brain tumors. The goal is to remove as much of the tumor as possible while maintaining neurological function. A biopsy may be done first to examine the types of cells the tumor is made of for a diagnosis. This is frequently done if the tumor is in an area with sensitive structures around it that may be injured if the whole tumor is surgically removed. | |
| 2. | Chemotherapy | |
| 3. | Radiation therapy | |
| 4. | Steroids (to treat and prevent swelling especially in the brain) | |
| 5. | Anti-seizure medication (to treat and prevent seizures associated with intracranial pressure) | |
| 6. | Placement of a ventriculoperitoneal shunt (Also called a VP shunt.) This is a tube that is placed into the fluid filled spaces of the brain called ventricles. The other end of the tube is placed into the abdomen to help drain excess fluid that can build up in the brain and cause an increase in pressure in the brain. | |
| 7. | Supportive care (to minimize the side effects of the tumor or treatment) | |
| 8. | Rehabilitation (to regain lost motor skills and muscle strength; speech, physical, and occupational therapists may be involved in the healthcare team) | |
| 9. | Antibiotics (to treat and prevent infections) | |
| 10. | Continuous follow-up care (to manage disease, detect recurrence of the tumor, and to manage late effects of treatment) |
Newer therapies that may be used to treat brain tumors include the following:
| 1. | Stereotactic Radiosurgery: A new technique that focuses high doses of radiation at the tumor site from many different angles, while sparing the surrounding normal tissue, with the use of photon beams from a linear accelerator or cobalt x-rays. | |
| 2. | Gene Therapy: A special gene is added to a virus that is injected into the brain tumor. An antivirus drug is then given which kills the cancer cells that have been infected with the altered virus. this is still considered an experimental treatment. | |
| 3. | Chemotherapy Wafers: Wafers containing a cancer-killing drug, BCNU, are inserted directly into the area of the brain tumor during surgery. | |
| 4. | Targeted Therapy: Newer drugs that are aimed at specific parts of tumor cells that help them grow. For example, a drug called bevacizumab affects a tumor's ability to make new blood vessels. It may be helpful for glioblastomas in adults. | |
| 5. | Electric Field Treatments: Electrodes are placed along the scalp to provide a mild electric current that may affect tumor cells more than normal brain cells. |
Long-term outlook for a person with a brain tumor:
Prognosis greatly depends on all of the following:
| 1. | Type of tumor | |
| 2. | Extent of the disease | |
| 3. | Size and location of the tumor | |
| 4. | Presence or absence of metastasis | |
| 5. | The tumor's response to therapy | |
| 6. | Your age, overall health, and medical history | |
| 7. | Your tolerance of specific medications, procedures, or therapies | |
| 8. | New developments in treatment |
As with any cancer, prognosis and long-term survival can vary greatly from individual to individual. Prompt medical attention and aggressive therapy are important for the best prognosis. Continuous follow-up care is essential for a person diagnosed with a brain tumor. Side effects of radiation and chemotherapy, as well as second malignancies, can occur in survivors of brain tumors.
Rehabilitation for lost motor skill and muscle strength may be required for an extended amount of time. Speech therapists and physical and occupational therapists may be involved in some form of rehabilitation. More research is needed to improve treatment, decrease side effects of the treatment for this disease, and develop a cure. New methods are continually being discovered to improve treatment and to decrease side effects.
Please consult your physician with any questions or concerns you may have regarding this condition.
Epilepsy and Seizures
What is Epilepsy?
Epilepsy is a neurological condition involving the brain that makes people more susceptible to having recurrent unprovoked seizures. It is one of the most common disorders of the nervous system and affects people of all ages, races and ethnic background.
Anything that interrupts the normal connections between nerve cells in the brain can cause a seizure; this includes a high fever, low blood sugar, alcohol or drug withdrawal, or a brain concussion. Under these circumstances, anyone can have one or more seizures. However, when a person has two or more unprovoked seizures, he or she is considered to have epilepsy. There are many possible causes of epilepsy, including an imbalance of nerve-signaling chemicals called neurotransmitters, tumors, strokes, and brain damage from illness or injury, or some combination of these. In the majority of cases, there may be no detectable cause for epilepsy.
What is a Seizure?
The brain is the center that controls and regulates all voluntary and involuntary responses in the body. It consists of nerve cells that normally communicate with each other through electrical activity. A seizure occurs when part(s) of the brain receives a burst of abnormal electrical signals that temporarily interrupts normal electrical brain function.
What are the different types of Seizures?
There are several different types of seizures, including the following:
A. Partial Seizures
Partial Seizures take place when abnormal electrical brain function occurs in one or more areas of one side of the brain. In about one-third of people with partial seizures, the person may experience an aura before the seizure occurs. An aura is a strange feeling, either consisting of visual changes, hearing abnormalities, or changes in the sense of smell. Two types of partial seizures include the following:
1. Simple Partial Seizures: The seizures typically last less than one minute. The person may show different symptoms depending upon which area of the brain is involved. If the abnormal electrical brain function is in the occipital lobe (the back part of the brain that is involved with vision), sight may be altered, but muscles are more commonly affected. The person's muscles are typically more commonly affected. The seizure activity is limited to an isolated muscle group, such as the fingers, or to larger muscles in the arms and legs. Consciousness is not lost in this type of seizure. The person may also experience sweating, nausea, or become pale.
2. Complex Partial Seizures: This type of seizure commonly occurs in the temporal lobe of the brain, the area of the brain that controls emotion and memory function. This seizure usually lasts between one to two minutes. Consciousness is usually lost during these seizures and a variety of behaviors can occur. These behaviors may range from gagging, lip smacking, running, screaming, crying, and/or laughing. When the person regains consciousness, the person may complain of being tired or sleepy after the seizure. This is called the postictal period.
B. Generalized Seizures
Generalized seizures involve both sides of the brain. There is loss of consciousness and a postictal state after the seizure occurs. Types of generalized seizures include the following:
1. Absence Seizures (formerly known as petit mal seizures): These seizures are characterized by an altered state of consciousness and staring episodes. Typically, the person's posture is maintained during the seizure. The mouth or face may move or the eyes may blink. The seizure usually lasts no longer than 30 seconds. When the seizure is over, the person may not recall what just occurred and may go on with his/her activities, acting as though nothing happened. These seizures may occur several times a day. This type of seizure is sometimes mistaken for a learning problem or behavioral problem. Absence seizures are uncommon before the age of 5 and occur more often in girls.
2. Atonic: With atonic seizures, there is a sudden loss of muscle tone and the person may fall from a standing position or suddenly drop his/her head. During the seizure, the person is limp and unresponsive.
3. Generalized Tonic-Clonic Seizures (GTC or formerly known as grand mal seizures): This seizure is characterized by five distinct phases that occur. The body, arms, and legs will flex (contract), extend (straighten out), and tremor (shake), followed by a clonic period (contraction and relaxation of the muscles) and the postictal period. During the postictal period, the person may be sleepy, have problems with vision or speech, and may have a bad headache, fatigue, or body aches.
4. Myoclonic Seizures: This type of seizure refers to quick movements or sudden jerking of a group of muscles. These seizures tend to occur in clusters, meaning that they may occur several times a day, or for several days in a row.
5. Infantile Spasms: This rare type of seizure disorder occurs in infants before six months of age. There is a high occurrence rate of this seizure when the child is awakening, or when he/she is trying to go to sleep. The infant usually has brief periods of movement of the neck, trunk, or legs that lasts for a few seconds. Infants may have hundreds of these seizures a day. This can be a serious problem, and can have long-term complications.
6. Febrile Seizures: This type of seizure is associated with fever. These seizures are more commonly seen in children between six months and six years of age, and there may be a family history of this type of seizure. Febrile seizures that last less than 15 minutes are called "simple," and typically do not have long-term neurological effects. Seizures lasting more than 15 minutes are called "complex" and there may be long-term neurological changes in the child.
What causes a seizure?
A person may experience one or many seizures. While the exact cause of the seizure may not be known, the more common seizures are caused by the following:
| 1. | in newborns and infants:  birth trauma birth trauma congenital (present at birth) problems congenital (present at birth) problems  fever fever metabolic or chemical imbalances in the body metabolic or chemical imbalances in the body |
|
| 2. | in children, adolescents, and adults: alcohol or drugs alcohol or drugs head trauma head trauma infectionr infectionr unknown reasons unknown reasons |
Other possible causes of seizures may include the following:
| 1. | brain tumor | |
| 2. | neurological problems | |
| 3. | drug withdrawal | |
| 4. | medications |
What are the Symptoms of a Seizure?
The person may have varying degrees of symptoms depending upon the type of seizure. The following are general symptoms of a seizure or warning signs of seizures. Symptoms or warning signs may include:
| 1. | staring | |
| 2. | jerking movements of the arms and largest | |
| 3. | stiffening of the body | |
| 4. | loss of consciousness | |
| 5. | breathing problems or breathing stops | |
| 6. | loss of bowel or bladder control | |
| 7. | falling suddenly for no apparent reason | |
| 8. | not responding to noise or words for brief periods | |
| 9. | appearing confused or in a haze | |
| 10. | sleepiness and irritability upon waking in the morning | |
| 11. | nodding the head | |
| 12. | periods of rapid eye blinking and staring |
During the seizure, the person's lips may become bluish and breathing may not be normal. The movements are often followed by a period of sleep or disorientation.
The symptoms of a seizure may resemble other problems or medical conditions. Always consult your physician for a diagnosis.
How are Seizures Diagnosed?
The full extent of the seizure may not be completely understood immediately after onset of symptoms, but may be revealed with a comprehensive medical evaluation and diagnostic testing. The diagnosis of a seizure is made with a physical examination and diagnostic tests. During the examination, the physician obtains a complete medical history of the person and family and asks when the seizures occurred. Seizures may be due to neurological problems and require further medical follow up.
Diagnostic tests may include:
| 1. | Blood Tests | |
| 2. | Electroencephalogram (EEG): A procedure that records the brain's continuous, electrical activity by means of electrodes attached to the scalp. | |
| 3. | Magnetic Resonance Imaging (MRI): A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. | |
| 4. | Computed Tomography Scan (Also called a CT or CAT scan.): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
| 5. | Lumbar Puncture (spinal tap): A special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. |
Treatment of a seizure:
Specific treatment for a seizure will be determined by your physician based on:
| 1. | your age, overall health, and medical history | |
| 2. | type of the seizure | |
| 3. | frequency of the seizures | |
| 4. | your tolerance for specific medications, procedures, or therapies | |
| 5. | expectations for the course of the condition | |
| 6. | your opinion or preference |
The goal of seizure management is to control, stop, or decrease the frequency of the seizures without interfering with the normal activities of daily living (ADLs). The major goals of seizure management include the following:
| 1. | proper identification of the type of seizure | |
| 2. | using medication specific to the type of seizure | |
| 3. | using the least amount of medication to achieve adequate control | |
| 4. | maintaining appropriate medication levels |
Treatment may include:
A. Medications
There are many types of medications used to treat seizures and epilepsy. Medications are selected based on the type of seizure, age of the patient, side effects, the cost of the medication, and the adherence with the use of the medication.
Medications used at home are usually taken by mouth (as capsules, tablets, sprinkles, or syrup), but some can be given rectally (into the person's rectum). If the person is in the hospital with seizures, medication by injection or intravenous (IV) may be used.
It is important to take your medication on time and as prescribed by your physician. Different people use up the medication in their body differently, so adjustments (schedule and dosage) may need to be made for the most effective seizure control.
All medications can have side effects, although some people may not experience side effects. Discuss your medication's side effects with your physician.
While you are taking medications, different tests may be done to monitor the effectiveness of the medication. These tests may include the following:
| 1. | Blood Work: Frequent blood draws testing is usually required to check the level of the medication in the body. Based on this level, the physician may increase or decrease the dose of the medication to achieve the desired level. This level is called the "therapeutic level" and is where the medication works most efficiently. Blood work may also be done to monitor the effects of medications on body organs. | |
| 2. | Urine Tests: These tests are performed to see how the person's body is responding to the medication. | |
| 3. | Electroencephalogram (EEG): An EEG is a procedure that records the brain's continuous, electrical activity by means of electrodes attached to the scalp. This test is done to monitor how the medication is helping the electrical problems in the brain. |
B. Vagus Nerve Stimulation (VNS)
Some people, whose seizures are not being well-controlled with seizure medications, may benefit from a procedure called vagus nerve stimulation (VNS). VNS is currently only used for persons over the age of 12 who have partial seizures that are not controlled by other methods.
VNS attempts to control seizures by sending small pulses of energy to the brain from the vagus nerve, which is a large nerve in the neck. This is done by surgically placing a small battery into the chest wall. Small wires are then attached to the battery and placed under the skin and around the vagus nerve. The battery is then programmed to send energy impulses every few minutes to the brain. When the person feels a seizure coming on, he/she may activate the impulses by holding a small magnet over the battery. In many cases, this will help to stop the seizure.
There are some side effects that may occur with the use of VNS. These may include, but are not limited to, the following:
| 1. | hoarseness | |
| 2. | Pain or discomfort in the throat | |
| 3. | change in voice |
C. Surgery
Another treatment option for seizures is surgery. Surgery may be considered in a person who:
| 1. | has seizures that are unable to be controlled with medications. | |
| 2. | has seizures that always start in one area of the brain. | |
| 3. | has a seizure in a part of the brain that can be removed without disrupting important behaviors such as speech, memory, or vision. |
Surgery for epilepsy and seizures is a very complicated surgery performed by a specialized surgical team. The operation may remove the part of the brain where the seizures are occurring, or, sometimes, the surgery helps to stop the spread of the bad electrical currents through the brain.
A person may be awake during the surgery. The brain itself does not feel pain. With the person awake and able to follow commands, the surgeons are better able to make sure that important areas of the brain are not damaged.
Surgery is not an option for everyone with seizures. Discuss this treatment option with your physician for more information.
More information regarding the person with seizures or epilepsy:
| 1. | Make sure you or your child (if age appropriate) understand the type of seizure that is occurring and the type of medication(s) that are needed. | |
| 2. | Know the dose, time, and side effects of all medications. | |
| 3. | Consult your physician before taking other medications. Medications for seizures can interact with many other medications, causing the medications to work improperly and/or causing side effects. | |
| 4. | Young women of childbearing age who are on seizure medications need to be informed that seizure medications are harmful to a fetus, and the medication may also decrease the effectiveness of oral contraceptives. | |
| 5. | Check with your state to understand any laws about people with epilepsy or seizures operating a motor vehicle. | |
| 6. | If a person has good control over the seizures, only minimal restrictions need to be placed on activities, in most cases. | |
| 7. | Specific follow-up will be determined by your physician. | |
| 8. | Medications for seizures may not be needed for the person's entire life. Some persons may be taken off their medications if they have been seizure-free for one to two years. This will be determined by your physician. |
Guillain-Barré Syndrome
What is Guillain-Barré syndrome?
Guillain-Barré syndrome is a neurological disorder in which the body's immune system attacks part of the peripheral nervous system. The onset can be quite sudden and unexpected. The disorder can develop over a few days, or it may take up to several weeks. A person experiences the greatest weakness within the first two weeks after symptoms appear.
Who is affected by Guillain-Barré syndrome?
Although rare, afflicting about one person in 100,000, Guillain-Barré syndrome can affect people at any age and both men and women equally. The disorder usually occurs a few days or weeks after a person has had symptoms of a respiratory or gastrointestinal viral infection. Occasionally, pregnancy, surgery, or vaccinations will trigger the syndrome.
What causes Guillain-Barré syndrome?
Currently, it is not known why Guillain-Barré strikes some people. What is known is that the body's immune system begins to attack the body itself.
Normally, the cells of the immune system attack only foreign material and invading organisms, but in Guillain-Barré syndrome, the immune system starts to destroy the myelin sheath that surrounds the axons of many nerve cells, and, sometimes, the axons themselves.
When this occurs, the nerves cannot send signals efficiently, the muscles lose their ability to respond to the commands of the brain, and the brain receives fewer sensory signals from the rest of the body. The result is an inability to feel heat, pain, and other sensations.
Guillain-Barré syndrome can occur after a viral infection, surgery, trauma, or a reaction to an immunization.
What are the symptoms of Guillain-Barré syndrome?
The following are the most common symptoms of Guillain-Barré syndrome. However each individual may experience symptoms differently.
The first symptoms include varying degrees of weakness or tingling sensations in the legs, which, sometimes, spreads to the arms and upper body. The symptoms may increase in severity until the following does or does not occur - in these cases, the disorder is considered a medical emergency:
 |
Muscles cannot be used at all | |
 |
The patient becomes nearly paralyzed | |
 |
It may become difficult to breathe | |
 |
Blood pressure and heart rate are affected |
Although symptoms can become life threatening, partial recovery is possible from even the most severe cases of Guillain-Barré syndrome. However, some degree of weakness may still be present. The symptoms of Guillain-Barré syndrome may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
How is Guillain-Barré syndrome diagnosed?
According to the National Institute of Neurological Disorders and Stroke (NINDS): Guillain-Barré is called a syndrome rather than a disease because it is not clear that a specific disease-causing agent is involved. A syndrome is a medical condition characterized by a collection of symptoms (what the patient feels) and signs (what a physician can observe or measure). The signs and symptoms of the syndrome can be quite varied, so physicians may, on rare occasions, find it difficult to diagnose Guillain-Barré in its earliest stages. Signs and symptoms that may differentiate Guillain-Barré from other disorders include the following. With Guillain-Barré:
 |
Symptoms appear on both sides of the body. | |
 |
Symptoms appear quickly - days or weeks as opposed to months. | |
 |
Reflexes are usually lost. | |
 |
Cerebral spinal fluid that bathes the spinal cord and brain contains more protein than usual. |
Other diagnostic procedures include the following:
 |
Spinal tap (also called a lumbar puncture) - a special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. | |
 |
Electrodiagnostic tests (i.e., electromyography (EMG) and nerve conduction velocity, or NCV) - studies that evaluate and diagnose disorders of the muscles and motor neurons. Electrodes are inserted into the muscle, or placed on the skin overlying a muscle or muscle group, and electrical activity and muscle response are recorded. |
Treatment for Guillain-Barré
Specific treatment for Guillain-Barré syndrome will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the syndrome | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the syndrome | |
 |
Your opinion or preference |
Currently, there is no known cure for Guillain-Barré syndrome. The goal of treatment is to prevent breathing problems and provide supportive care (relief of symptoms). Medications are used to control pain and other conditions that may be present. In addition, treatments such as plasmapheresis or immunoglobulin administration may be used to suppress the immune system and/or reduce inflammation caused by the immune system’s response to the disease.
Plasmapheresis is a procedure which removes the plasma (liquid part of the blood) and replaces it with other fluids. Antibodies are also removed with the plasma, which is thought to help reduce the symptoms of the disease. Another treatment is the administration of immunoglobulin, a blood product that helps to decrease the immune system’s attack on the nervous system.
Other therapies include hormonal therapy and physical therapy (to increase muscle flexibility and strength).
Through research, new treatments for Guillain-Barré syndrome are continually being identified.
Head Injury
What is a Head Injury?
Head injuries are one of the most common causes of disability and death in adults. The injury can be as mild as a bump, bruise (contusion), or cut on the head, or can be moderate to severe in nature due to a concussion, deep cut or open wound, fractured skull bone(s), or from internal bleeding and damage to the brain.
A head injury is a broad term that describes a vast array of injuries that occur to the scalp, skull, brain, and underlying tissue and blood vessels in the head. Head injuries are also commonly referred to as brain injury, or traumatic brain injury (TBI), depending on the extent of the head trauma.
Head injuries are rising dramatically, with around 1.47 million injured per year - about 52,000 of those dying. Five million Americans are alive today who have had a head injury and now need help with the activities of daily living, costing the country more than $56 billion per year.
What are the different types of Head Injury?
The following are some of the different types of head injuries:
A. Concussion: A concussion is an injury to the head area that may cause instant loss of awareness or alertness for a few minutes up to a few hours after the traumatic event.
B. Skull Fracture:A skull fracture is a break in the skull bone. There are four major types of skull fractures, including the following:
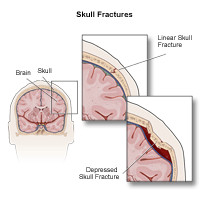
| 1. | Linear Skull FracturesThis is the most common type of skull fracture. In a linear fracture, there is a break in the bone, but it does not move the bone. These patients may be observed in the hospital for a brief amount of time, and can usually resume normal activities in a few days. Usually, no interventions are necessary. | |
| 2. | Depressed Skull FracturesThis type of fracture may be seen with or without a cut in the scalp. In this fracture, part of the skull is actually sunken in from the trauma. This type of skull fracture may require surgical intervention, depending on the severity, to help correct the deformity. | |
| 3. | Diastatic Skull FracturesThese are fractures that occur along the suture lines in the skull. The sutures are the areas between the bones in the head that fuse when we are children. In this type of fracture, the normal suture lines are widened. These fractures are more often seen in newborns and older infants. | |
| 4. | Basilar Skull FractureThis is the most serious type of skull fracture, and involves a break in the bone at the base of the skull. Patients with this type of fracture frequently have bruises around their eyes and a bruise behind their ear. They may also have clear fluid draining from their nose or ears due to a tear in part of the covering of the brain. These patients usually require close observation in the hospital. | |
| 5. | Intracranial hematoma (ICH)There are several types of ICH, or blood clots, in or around the brain. The different types are classified by their location in the brain. These can range from mild head injuries to quite serious and potentially life-threatening injuries. The different types of ICH include the following: |
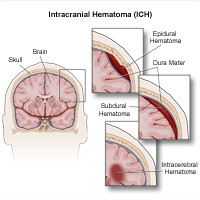
 |
Epidural Hematoma: Epidural hematomas occur when a blood clot forms underneath the skull, but on top of the dura, the tough covering that surrounds the brain. They usually come from a tear in an artery that runs just under the skull called the middle meningeal artery. Epidural hematomas are usually associated with a skull fracture. | |
 |
Subdural Hematoma: Subdural hematomas occur when a blood clot forms underneath the skull and underneath the dura, but outside of the brain. These can form from a tear in the veins that go from the brain to the dura, or from a cut on the brain itself. They are sometimes, but not always, associated with a skull fracture. | |
 |
Contusion or Intracerebral Hematoma: A contusion is a bruise to the brain itself. A contusion causes bleeding and swelling inside of the brain around the area where the head was struck. Contusions may occur with skull fractures or other blood clots such as a subdural or epidural hematoma. When bleeding occurs inside the brain itself (also called "intraparenchymal hemmorage"), this can sometimes occur spontaneously. When trauma is not the cause, the most common causes are long-standing high blood pressure in older adults, bleeding disorders in either children or adults, or the use of medications that cause blood thinning or certain drugs of abuse. | |
 |
Diffuse Axonal Injury (DAI): These injuries are fairly common and are usually caused by shaking of the brain back and forth, which can happen in car accidents, from falls or shaken baby syndrome. Diffuse injuries can be mild, such as with a concussion, or may be very severe, as in diffuse axonal injury (DAI). In DAI, the patient is usually in a coma for a prolonged period of time, with injury to many different parts of the brain. |
What causes a Head Injury?
There are many causes of head injury in children and adults. The most common traumatic injuries are from motor vehicle accidents (sutomobiles, motorcycles, or struck as a pedestrian), from violence, from falls, or as a result of child abuse. Subdural hematomas and brain hemmorages (the so-called "intraparenchymal hemmorages") can sometimes happen spontaneaously.
What causes bruising and internal damage to the brain?
When there is a direct blow to the head, shaking of the child (as seen in many cases of child abuse), or a whiplash-type injury (as seen in motor vehicle accidents), the bruising of the brain and the damage to the internal tissue and blood vessels is due to a mechanism called coup-countrecoup. A bruise directly related to trauma, at the site of impact, is called a coup lesion (pronounced COO). As the brain jolts backwards, it can hit the skull on the opposite side and cause a bruise called a countrecoup lesion. The jarring of the brain against the sides of the skull can cause shearing (tearing) of the internal lining, tissues, and blood vessels that may cause internal bleeding, bruising, or swelling of the brain.
What are the Symptoms of a Head Injury?
The person may have varying degrees of symptoms associated with the severity of the head injury. The following are the most common symptoms of a head injury. However, each individual may experience symptoms differently. Symptoms may include:
A. Mild Head Injury:
 |
Raised, swollen area from a bump or a bruise | |
 |
Small, superficial (shallow) cut in the scalp | |
 |
Headache | |
 |
Sensitivity to noise and light | |
 |
Irritability | |
 |
Confusion | |
 |
Lightheadedness and/or dizziness | |
 |
Problems with balance | |
 |
Nausea | |
 |
Problems with memory and/or concentration | |
 |
Change in sleep patterns | |
 |
Blurred vision | |
 |
"Tired"eyes | |
 |
Ringing in the ears (tinnitus) | |
 |
Alteration in taste | |
 |
Fatigue/lethargy |
B. Moderate to severe head injury (requires immediate medical attention) - symptoms may include any of the above plus:
 |
Loss of consciousness | |
 |
Severe headache that does not go away | |
 |
Repeated nausea and vomiting | |
 |
Loss of short-term memory, such as difficulty remembering the events that led right up to and through the traumatic event | |
 |
Slurred speech | |
 |
Difficulty with walking | |
 |
Weakness in one side or area of the body | |
 |
Sweating | |
 |
Pale skin color | |
 |
Seizures or convulsions | |
 |
Behavior changes including irritability | |
 |
Blood or clear fluid draining from the ears or nose | |
 |
One pupil (dark area in the center of the eye) looks larger than the other eye | |
 |
Deep cut or laceration in the scalp | |
 |
Open wound in the head | |
 |
Foreign object penetrating the head | |
 |
Coma (a state of unconsciousness from which a person cannot be awakened; responds only minimally, if at all, to stimuli; and exhibits no voluntary activities) | |
 |
Vegetative state (a condition of brain damage in which a person has lost his thinking abilities and awareness of his surroundings, but retains some basic functions such as breathing and blood circulation) | |
 |
Locked-in syndrome (a neurological condition in which a person is conscious and can think and reason, but cannot speak or move) |
The symptoms of a head injury may resemble other problems or medical conditions. Always consult your physician for a diagnosis.
How are head injuries diagnosed?
The full extent of the problem may not be completely understood immediately after the injury, but may be revealed with a comprehensive medical evaluation and diagnostic testing. The diagnosis of a head injury is made with a physical examination and diagnostic tests. During the examination, the physician obtains a complete medical history of the patient and family and asks how the injury occurred. Trauma to the head can cause neurological problems and may require further medical follow up.
Diagnostic tests may include:
 |
Blood tests | |
 |
X-ray - a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. | |
 |
Computed tomography scan (Also called a CT or CAT scan.) - a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
 |
Electroencephalogram (EEG) - a procedure that records the brain's continuous, electrical activity by means of electrodes attached to the scalp. | |
 |
Magnetic resonance imaging (MRI) - a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. |
Treatment of a head injury:
Specific treatment of a head injury will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the head injury | |
 |
Type of head injury | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the head injury | |
 |
Your opinion or preference |
Depending on the severity of the injury, treatment may include:
 |
Ice | |
 |
Rest | |
 |
Topical antibiotic ointment and adhesive bandage | |
 |
Observation | |
 |
Immediate medical attention | |
 |
Stitches | |
 |
Hospitalization for observation | |
 |
Moderate sedation or assistance with breathing that would require being placed on a breathing machine, or mechanical ventilator or respirator | |
 |
Surgery |
Treatment is individualized, depending on the extent of the condition and the presence of other injuries. If the patient has a severe head injury, he/she may require monitoring for increased intracranial pressure (pressure inside the skull). Head injury may cause the brain to swell. Since the brain is covered by the skull, there is only a small amount of room for it to swell. This causes pressure inside the skull to increase, which can lead to brain damage.
How is ICP monitored?
Intracranial pressure is measured in two ways. One way is to place a small hollow tube (catheter) into the fluid-filled space in the brain (ventricle). Other times, a small, hollow device (bolt) is placed through the skull into the space just between the skull and the brain. Both devices are inserted by the physician either in the intensive care unit (ICU) or in the operating room. The ICP device is then attached to a monitor that gives a constant reading of the pressure inside the skull. If the pressure goes up, it can be treated right away. While the ICP device is in place the patient will be given medication to stay comfortable. When the swelling has gone down and there is little chance of more swelling, the device will be removed.
Life-long considerations for a person with a head injury:
The key is to promote a safe environment for children and adults and to prevent head injuries from occurring. The use of seat belts when riding in the car and helmets (when worn properly) for activities such as bicycle riding, in-line skating, and skateboarding may protect the head from sustaining severe injuries. Persons who suffer a severe brain injury may lose part(s) of muscle, speech, vision, hearing, or taste function, depending on the area of brain damage. Long- or short-term changes in personality or behavior may also occur. These persons require long-term medical and rehabilitative (physical, occupational, or speech therapy) management. The extent of the person's recovery depends upon the type of brain injury and other medical problems that may be present. It is important to focus on maximizing the person's capabilities at home and in the community. Positive reinforcement will encourage the patient to strengthen his/her self-esteem and promote independence
Headache
What is a Headache?
A headache is pain or discomfort in the head or face area. Headaches vary greatly in terms of pain location, pain intensity, and how frequently they occur. As a result of this variation, several categories of headache have been created by the International Headache Society (IHS) to more precisely define specific types of headaches.
What aches when you have a Headache?
There are several areas in the head that can hurt when you have a headache, including the following:
 |
A network of nerves that extends over the scalp | |
 |
Certain nerves in the face, mouth, and throat | |
 |
Muscles of the head | |
 |
Blood vessels found along the surface and at the base of the brain (these contain delicate nerve fibers) |
The tissues of the brain itself do not hurt because they do not have pain-sensitive nerve fibers.
What causes a Headache?
Headaches may be caused by a number of conditions, such as disorders of the neck, eyes, brain, jaw, or teeth. Headaches with an underlying medical condition are classified as secondary headaches because they are related to the condition. An example of this would be a headache due to neck injury or sinus infection.
Other headaches are classified as primary because the headache itself is the main medical problem, although underlying non-medical causes, such as muscle tension or foods, may be identified. Other contributing factors may include medications, dehydration, or changing levels of hormones. These factors that influence headaches are sometimes called headache triggers.
What are some of the different types of Primary Headaches?
A. Migraines
This type of headache is distinguished by the fact that symptoms other than pain occur as part of the headache. Nausea and vomiting, lightheadedness, sensitivity to light (photophobia), and other visual symptoms typically occur.
Migraines are also unique in that they have distinct phases. Not all individuals experience each phase, however. The phases of a migraine headache may include:
| 1. | Premonition Phase: A change in mood or behavior that may occur hours or days before the headache. | |
| 2. | Aura Phase: A group of visual, sensory, or motor symptoms that immediately precede the headache. Examples include hallucinations, numbness, changes in speech, and muscle weakness. | |
| 3. | Headache Phase: Period during the actual headache with throbbing pain on one or both sides of the head. Sensitivity to light and motion are common, as are depression, fatigue, and anxiety. | |
| 4. | Headache Resolution Phase: Pain lessens during this phase, but may be replaced with fatigue, irritability, and difficulty concentrating. Some individuals feel refreshed after an attack, while others do not. |
B. Tension Headaches
Tension headaches are the most common type of headache. Stress and muscle tension are often factors in tension-type headaches. While symptoms may differ, the following are common symptoms of a tension-type headache:
| 1. | Slow onset of the headache | |
| 2. | Head usually hurts on both sides | |
| 3. | Pain is dull or feels like a band or vice around the head | |
| 4. | Pain may involve the back (posterior) part of the head or neck | |
| 5. | Pain is mild to moderate, but not severe |
Tension type headaches typically do not cause nausea, vomiting, or sensitivity to light (photophobia).
C. Cluster Headaches
Cluster headaches usually occur in a series that may last weeks or months, and the headache series may return every year or two. While people often experience symptoms differently, the following are the most common symptoms of a cluster headache:
| 1. | Severe pain on one side of the head, usually behind one eye | |
| 2. | The eye that is affected may have a droopy lid, small pupil, or redness and swelling of the eyelid | |
| 3. | Runny nose or congestion | |
| 4. | Swelling of the forehead |
What are the most serious Symptoms of a Headache?
Headache symptoms depend upon the type of headache. The frequency of headaches and the intensity of the symptoms may vary as well. Symptoms that may suggest a more serious headache include any of the following:
 |
Headaches that start early in the morning | |
 |
Pain that is worsened by strain, such as a cough or a sneeze | |
 |
Vomiting without nausea | |
 |
Sudden onset of pain and the "worst headache" ever | |
 |
Headache that is becoming more severe or continuous | |
 |
Personality changes | |
 |
Changes in vision | |
 |
Weakness in the arms or legs | |
 |
Seizures or epilepsy |
The symptoms of a headache may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How are headaches diagnosed?
The full extent of the problem may not be understood immediately, but may be revealed with a comprehensive medical evaluation and diagnostic testing. The diagnosis of a headache is made with a careful history, physical examination and diagnostic tests.
Questions commonly asked during the exam may include, but are not limited to, the following:
 |
When do headaches occur? | |
 |
What is the location of the headache? | |
 |
What do the headaches feel like? | |
 |
How long do the headaches last? | |
 |
Headache that is becoming more severe or continuous | |
 |
Do changes in position or sitting up cause the headache? | |
 |
Do you have trouble sleeping? | |
 |
Do you have a history of stress? | |
 |
Is there a history of head injury? |
If the history is consistent with migraine or tension-type headaches and the neurological exam is normal, no further diagnostic testing may be necessary. However, if it is not a primary type headache, then other tests may be needed to determine the cause.
Tests used to determine the cause of a headache may include:
 |
Blood Tests: Various blood chemistry and other laboratory tests may be run to check for underlying conditions. | |
 |
Sinus x-rays: A diagnostic imaging procedure to evaluate for congestion or other problems that may be corrected. | |
 |
Magnetic Resonance Imaging (MRI) - A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. | |
 |
Computed tomography scan (Also called a CT or CAT scan): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. |
Treatment for headaches:
Specific treatment for headaches will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Type of headaches | |
 |
Severity and frequency of the headaches | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Your opinion or preference |
The ultimate goal of treatment is to stop headaches from occurring. Adequate headache management depends on the accurate identification of the type of headache and may include:
 |
Avoiding known triggers, such as certain foods and beverages, lack of sleep, and fasting | |
 |
Changing eating habits | |
 |
Exercise | |
 |
Resting in a quiet, dark environment | |
 |
Medications, as recommended by your physician | |
 |
Stress management |
Migraine headaches may require specific medication management including:
 |
Abortive Medications: Medications, prescribed by your physician, that act on specific receptors in nerves and blood vessels in the head to stop a headache in progress. | |
 |
Rescue Medications: Medications purchased over-the-counter, such as analgesics (pain relievers), to stop the headache. | |
 |
Preventive Medications: Medications, prescribed by your physician, that are taken daily to reduce the onset of severe migraine headaches. |
Some headaches may require immediate medical attention including hospitalization for observation, diagnostic testing, or even surgery. Treatment is individualized depending on the underlying condition causing the headache. Full recovery depends on the type of headache and other medical problems that may be present.
Lumbar Disc Disease (Herniated Disc)

Anatomy of the Lumbar Spine:
The vertebral column, also called the backbone, is made up of 33 vertebrae that are separated by spongy disks and classified into four distinct areas. The cervical area consists of seven bony parts in the neck; the thoracic spine consists of 12 bony parts in the back area; the lumbar spine consists of five bony segments in the lower back area; five sacral bones (fused into one bone, the sacrum); and four coccygeal bones (fused into one bone, the coccyx).
Lumbar disc disease occurs in the lumbar area of the spine. The lumbar area of the spine (and other areas of the spine) is made up of two parts, including the following:
| A. | Vertebral Bodies: The parts that are made of bone. | |
| B. | Intervertebral Discs: Also known as the discs; the discs are located between the bony parts of the spine and act as "shock absorbers" for the spine. |
The vertebral bodies are numbered from 1 to 5 in the lumbar spine and the discs are located between two of the vertebral bodies and are numbered accordingly (such as a disc at L2-3, or between the lumbar discs numbered 2 and 3).
The Intervertebral disc is composed of two parts, including the following:
| 1. | Annulus Fibrosis: A tough outer ring of fibrous tissue. | |
| 2. | Nucleus Pulposus: Located inside the annulus fibrosis; a more gelatinous or soft material. |
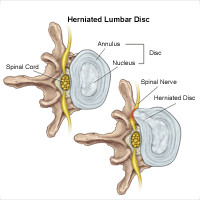
What is Lumbar Disc Disease (herniated disc, ruptured disc or bulging disc)?
As we age, the intervertebral disc may lose water and become dried out. As this happens, the disc compresses. This may lead to the deterioration of the tough outer ring allowing the nucleus, or the inside of the ring, to bulge out. This is considered a bulging disc.
As the disc continues to degenerate, or with continued stress on the spine, the inner nucleus pulposus may actually rupture out from the annulus. This is considered a ruptured, or herniated, disc. The fragments of disc material can then press on the nerve roots that are located just behind the disc space. This can cause pain, weakness, numbness, or changes in sensation.
Most disc herniations happen at the lower lumbar spine, especially at the L4-5 and L5-S1 levels.
What causes Lumbar Disc Disease?
Lumbar disc disease is due to a change in the structure of the normal disc. Most of the time, disc disease comes as a result of aging and the degeneration that occurs within the disc. Occasionally, severe trauma can cause a normal disc to herniate. Trauma may also cause an already herniated disc to worsen.
What are the Symptoms of Lumbar Disc Disease?
The symptoms of lumbar disc disease vary depending on where the disc has herniated, and what nerve root it is pushing on. The following are the most common symptoms of lumbar disc disease. However, each individual may experience different symptoms. Symptoms may include:
 |
intermittent or continuous back pain (this may be made worse by movement, coughing, sneezing, or standing for long periods of time) | |
 |
spasm of the back muscles | |
 |
sciatica - pain that starts near the back or buttock and travels down the leg to the calf or into the foot. | |
 |
muscle weakness in the legs | |
 |
numbness in the leg or foot | |
 |
decreased reflexes at the knee or ankle | |
 |
changes in bladder or bowel function |
The symptoms of lumbar disc disease may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is Lumbar Disc Disease diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for lumbar disc disease may include the following:
 |
x-ray: A diagnostic test which uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. | |
 |
Magnetic Resonance Imaging (MRI): A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. | |
 |
Myelogram: A procedure that uses dye injected into the spinal canal to make the structure clearly visible on x-rays. | |
 |
Computed Tomography Scan (Also called a CT or CAT scan.): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
 |
Electromyography (EMG): A diagnostic test that measures muscle response or electrical activity in response to a nerve’s stimulation of the muscle |
Treatment for Lumbar Disc Disease:
Specific treatment for lumbar disc disease will be determined by your physician based on:
 |
your age, overall health, and medical history | |
 |
extent of the condition | |
 |
type of condition | |
 |
your tolerance for specific medications, procedures, or therapies | |
 |
expectations for the course of the condition | |
 |
your opinion or preference |
Typically, conservative therapy is the first line of treatment to manage lumbar disc disease. This may include a combination of the following:
 |
bed rest | |
 |
patient education on proper body mechanics (to help decrease the chance of worsening pain or damage to the disc) | |
 |
physical therapy, which may include ultrasound, massage, conditioning, and exercise programs | |
 |
weight control | |
 |
use of a lumbosacral back support | |
 |
medications (to control pain and/or to relax muscles) |
When these conservative measures fail, surgery for removal of a herniated disc may be recommended. Surgery is done under general anesthesia. An incision is placed in the lower back over the area where the disc is herniated. Some bone from the back of the spine may be removed to gain access to the area where the disc is located. Typically, the herniated part of the disc and any extra loose pieces of disc are removed from the disc space.
After surgery, restrictions may be placed on the patient's activities for several weeks while healing is taking place to prevent another disc herniation from occurring. Your physician will discuss any restrictions with you.
There are other experimental therapies that are being used to treat lumbar disc disease. Discuss these treatment options with your physician.
Meningitis
What is Meningitis?
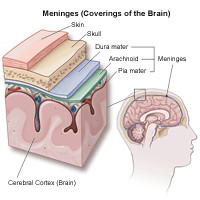
Meningitis is an inflammation of the meninges, the membranes that surround the brain. There are three meninges, including the following:
| 1. | Dura Mater: The outside membrane that adheres to the inside of the skull. | |
| 2. | Arachnoid: The middle membrane. | |
| 3. | Pia mater: The innermost membrane, which adheres to the brain. |
What Causes Meningitis?
There are two distinct types of meningitis, each with different causes:
| Viral: caused by a virus |
|
||||||||||||
| Bacterial : Caused by a bacterium |
|
||||||||||||
| Types |
|
How does the infection reach the brain?
The infection can reach the brain via several different routes, including through the bloodstream from another infected part of the body, through the bones of the skull from infected sinuses or inner ears, or from a head injury, such as a fractured skull or penetrating wound. In particular, this occurs when the body's resistance is compromised by certain factors such as following surgery or an extended hospitalization, a weakened immune system, or as a result of chronic kidney failure.
What are the Symptoms of Meningitis?
The following are the most common symptoms of meningitis. However, each individual may experience symptoms differently. Symptoms may include:
 |
Fever | |
 |
Headache | |
 |
Nausea and vomiting | |
 |
Stiff neck | |
 |
Photophobia (low tolerance to bright light) Confusion | |
 |
Joint aches or pains | |
 |
Drowsiness | |
 |
Seizures |
Symptoms for children may also include:
 |
Fever | |
 |
High-pitched cry | |
 |
Pale, blotchy skin color | |
 |
Not wanting to eat | |
 |
Vomiting | |
 |
Fretful and fussy | |
 |
Arching back | |
 |
Difficult to wake |
It is important to note that these symptoms may not occur all at once, nor in everyone who contracts meningitis. The symptoms of meningitis may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is Meningitis Diagnosed?
In addition to a complete medical history and physical examination, diagnostic procedures for meningitis may include the following:
 |
Lumbar Puncture (spinal tap): A special needle is placed into the lower back, into the spinal canal. This is the area around the spinal cord. The pressure in the spinal canal and brain can then be measured. A small amount of cerebral spinal fluid (CSF) can be removed and sent for testing to determine if there is an infection or other problems. CSF is the fluid that bathes the brain and spinal cord. | |
 |
Blood Testing | |
 |
Computed Tomography Scan (Also called a CT or CAT scan.): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. |
Treatment for Meningitis:
Specific treatment for meningitis will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
The organism that is causing the infection | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
Treatment may include:
 |
Bacterial Meningitis:Treatment for bacterial meningitis usually involves intravenous (IV) antibiotics. The earlier the treatment is initiated, the better the outcome. While steroid administration has been shown to be helpful in treating bacterial meningitis in infants and children, this treatment is used less frequently in adults. Dexamethasone, a type of steroid, may be given in more acute cases of bacterial meningitis, to decrease the inflammatory response caused by the bacteria. |
|
 |
Viral Meningitis: Treatment for viral meningitis is usually supportive (aimed at relieving symptoms). With the exception of the herpes simplex virus, there are no specific medications to treat the organisms that cause viral meningitis. Sometimes antiviral medications are used to combat some other specific types of viruses, with variable benefit. | |
 |
Fungal Meningitis: An intravenous anti-fungal medication may be administered to treat fungal meningitis. | |
 |
Tuberculous (TB) meningitis: A long course (one year) of medications is recommended for persons who develop TB meningitis. The therapy usually involves treatment with several different medications for the first few months, followed by other medications. |
What is Supportive Therapy for Meningitis?
While a person is recovering from meningitis, other therapies may be initiated to improve healing and comfort, and provide relief from symptoms. These may include the following:
 |
Bed rest | |
 |
Medications (to reduce fever and headache) |
In addition, supplemental oxygen or mechanical ventilation (respirator) may be required if you become very ill and have difficulty breathing.
Prevention of meningitis:
Several vaccines are currently available to prevent some of the bacterial organisms that can cause meningitis. However, routine vaccination with these vaccines is recommended primarily for infants and children.
In certain conditions, your physician may recommend one of the meningitis vaccines. These conditions may include, but are not limited to, the following:
 |
Chronic lung conditions, such as emphysema or COPD | |
 |
Heart disease | |
 |
Diabetes | |
 |
Chronic renal (kidney) failure | |
 |
Travel to countries where meningitis is prevalent | |
 |
Decreased immunity status | |
 |
Certain blood disorders |
If you have questions regarding prevention, consult your physician.
Multiple Sclerosis
Multiple Sclerosis
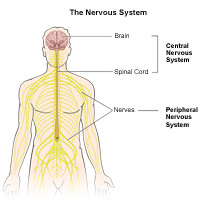
Multiple sclerosis (MS) is a chronic disease of the central nervous system. It is thought to be an autoimmune disorder. It is an unpredictable condition that can be relatively benign, disabling, or devastating. Some individuals with MS may be mildly affected while others may lose their ability to see clearly, write, speak, or walk when communication between the brain and other parts of the body becomes disrupted.
Myelin is a fatty tissue that surrounds and protects the nerve fibers. Myelin is lost in multiple areas with MS. This loss of myelin forms scar tissue called sclerosis. These areas are also called plaques or lesions. When damaged in this way, the nerves are unable to conduct electrical impulses to and from the brain.
What causes Multiple Sclerosis?
There are many possible causes of MS, including the following:
 |
Viruses | |
 |
Autoimmune disorders | |
 |
Environmental factors | |
 |
Genetic factors |
However, not enough is known about the role these factors play to definitively describe why a particular patient develops MS.
What are the symptoms of MS?
The symptoms of MS are erratic. They may be mild or severe, of long duration or short. They may appear in various combinations, depending on the area of the nervous system affected. The following are the most common symptoms of MS. However, each individual may experience symptoms differently. Symptoms may include:
A. Initial symptoms of MS
The following are often initial symptoms of MS:
 |
Blurred or double vision | |
 |
Red-green color distortion | |
 |
Pain and loss of vision due to optic neuritis, an inflammation of the optic nerve | |
 |
Difficulty walking | |
 |
Paresthesia - abnormal sensation, or pain, such as numbness, prickling, or "pins and needles." |
B. Other symptoms of Multiple Sclerosis
Throughout the course of the illness, an individual may experience any/all of the following symptoms, to a varying degree:
 |
Muscle weakness in the extremities | |
 |
Difficulty with coordination (impaired walking or standing may result; partial or complete paralysis is possible) | |
 |
Spasticity - the involuntary increased tone of muscles leading to stiffness and spasms. | |
 |
Fatigue (this may be triggered by physical activity, but may subside with rest; constant, persistent fatigue is possible) | |
 |
Loss of sensation | |
 |
Speech impediments | |
 |
Tremor | |
 |
Dizziness | |
 |
Hearing loss | |
 |
Bowel and bladder disturbances | |
 |
Depression | |
 |
Changes in Sexual function |
Approximately 50 percent of all people with MS experience cognitive impairments related to their disease. The effects of these impairments may be mild, often detectable only after comprehensive testing, and may include difficulty with any/all of the following:
 |
Concentrationn | |
 |
Attention | |
 |
Memory | |
 |
Poor judgment |
Symptom categories of MS:
Primary symptoms: A direct result of demyelination, the destruction of myelin (the fatty sheath that surrounds and insulates nerve fibers in the central nervous system) may result in the following:
|
Secondary symptoms : Complications that arise as a result of the primary symptoms, for example:
|
Tertiary symptoms: The social, vocational, and psychological complications of the primary and secondary symptoms, for example:
|
The symptoms of MS may resemble other medical conditions or problems. Always consult your physician for a diagnosis.
How is Multiple Sclerosis diagnosed?
With today's medicine, there is no definitive test available to diagnose multiple sclerosis. However, a probable diagnosis can be made by following a careful process which demonstrates findings that are consistent with MS, that also rule out other causes and diseases.
What are the two criteria used when diagnosing MS?
 |
There must have been two attacks at least one month apart. An attack is a sudden appearance of or worsening of any MS symptom or symptoms that lasts at least 24 hours. | |
 |
There must be more than one area of damage to the central nervous system myelin, the sheath that surrounds and protects nerve fibers, which must have occurred at more than one point in time and was not caused by any other disease. | |
 |
More commonly nowadays, a single attack together with certain patterns of changes in brain tissue seen on a magnetic resonance image (MRI) of the brain [see the description of this below] can strongly suggest the diagnosis of MS. |
What does an evaluation for MS cover?
Evaluation for MS involves a complete medical history and neurological exam, which includes:
 |
Mental functions | |
 |
Emotional functions | |
 |
Language functions | |
 |
Movement and coordination | |
 |
Vision | |
 |
Balance | |
 |
Functions of the five senses |
Evaluation procedures for MS:
The following may be used when evaluating for multiple sclerosis:
 |
Magnetic Resonance Imaging (MRI): A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body; to detect the presence of plaques or scarring caused by MS. | |
 |
Evoked Potentials: Procedures that record the brain's electrical response to visual, auditory, and sensory stimuli; to show if there is a slowing of messages in the various parts of the brain. | |
 |
Cerebral Spinal Fluid Analysis (also called spinal tap or lumbar puncture): A procedure used to make an evaluation or diagnosis by examining the fluid withdrawn from the spinal column; to check for cellular and chemical abnormalities associated with MS. | |
 |
Blood tests (to rule out other causes for various neurological symptoms): Evaluation and diagnosis of MS requires a variety of tools to rule out other possible disorders and a series of laboratory tests that, if positive, confirms the diagnosis. |
Treatment for MS:
Specific treatment for MS will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
Treatments for the conditions associated with MS may include the following:
 |
Medication | |
 |
Clinical trials | |
 |
Assistive technology | |
 |
Rehabilitation activities |
There is no cure yet for MS. However, there are strategies to modify the disease course, treat exacerbations, manage symptoms, and improve function and mobility.
Rehabilitation for people with MS:
Rehabilitation varies depending upon the range, expression, severity, and progression of symptoms. MS rehabilitation may help to accomplish the following:
 |
Restore functions that are essential to the activities of daily living (ADLs) | |
 |
Help the patient to reach maximum independence | |
 |
Promote family involvement | |
 |
Empower the patient to make the appropriate decisions relating to his/her care | |
 |
Educate the patient regarding the use of assistive devices (i.e., canes, braces, walkers) | |
 |
Establish an appropriate exercise program that promotes muscle strength, endurance, and control | |
 |
Reestablish motor skills | |
 |
Improve communication skills for patients who have difficulty speaking because of weakness or incoordination of face and tongue muscles | |
 |
Manage bowel or bladder incontinence | |
 |
Provide cognitive retraining | |
 |
Adapt the home environment to emphasize function, safety, accessibility, and mobility |
Muscular Dystrophy
What is Muscular Dystrophy?
Muscular dystrophy (MD) is a broad term that describes a genetic (inherited) disorder of the muscles. Muscular dystrophy causes the muscles in the body to become very weak. The muscles break down and are replaced with fatty deposits over time.
Other health problems commonly associated with muscular dystrophy include the following:
 |
Heart Problems | |
 |
scoliosis: A lateral, or sideways, curvature and rotation of the back bones (vertebrae), giving the appearance that the person is leaning to one side. | |
 |
Obesity |
Some forms of MD first appear in infancy or early to late childhood, while others may not appear until adolescence, middle-age, or later.The most common forms of muscular dystrophy are Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy. The two forms are very similar, but Becker muscular dystrophy is less severe than DMD. Girls are rarely affected by either of these two forms of muscular dystrophy.
What causes muscular dystrophy?
Duchenne muscular dystrophy is a genetic disease which means it is inherited. Our genes determine our traits, such as eye color and blood type. Genes are contained in the cells of our bodies on stick-like structures called chromosomes. There are normally 46 chromosomes in each cell of our body, or 23 pairs. The first 22 pairs are shared in common between males and females, while the last pair determine gender and are called the sex chromosome pair: females have two X chromosomes, while males have one X and one Y chromosome.
Duchenne muscular dystrophy is caused by an X-linked recessive gene. "X-linked" means that the gene causing the trait or the disorder is located on the X chromosome. Genes on the X chromosome can be recessive or dominant, and their expression in females and males is not the same because the genes on the Y chromosome do not exactly pair up with the genes on the X. X-linked recessive genes are expressed in females only if there are two copies of the gene (one on each X chromosome). However, for males there only needs to be one copy of an X-linked recessive gene in order for the trait or disorder to be expressed. For example, a woman can carry a recessive gene on one of the X chromosomes unknowingly, and pass it on to a son, who will express the trait or disease.

Therefore, half of the daughters have the gene and can pass it to the next generation. The other half do not have the gene and therefore cannot pass it on. Half of the sons do not have the gene and cannot pass it on. The other half of the sons have inherited the gene and will express the trait or disorder (in this case, DMD).
What are the Symptoms of Muscular Dystrophy?
Muscular dystrophy is usually diagnosed in children between 3 and 6 years of age. Early signs of the illness include a delay in walking, difficulty rising from a sitting or lying position, and frequent falling, with weakness typically affecting the shoulder and pelvic muscle as one of the initial symptoms. The following are the most common symptoms of muscular dystrophy. However, each individual may experience symptoms differently. Symptoms may include:
 |
clumsy movement | |
 |
difficulty climbing stairs | |
 |
frequently trips and falls | |
 |
unable to jump or hop normally | |
 |
tip toe walking | |
 |
leg pain | |
 |
facial weakness | |
 |
inability to close eyes or whistle | |
 |
shoulder and arm weakness |
A tell-tale clinical characteristic for Duchenne muscular dystrophy (DMD) is Gowers' sign. Children with Duchenne muscular dystrophy find it very hard to get up from a sitting or lying position on the floor. They first pull up to their hands and knees. The child walks his/her hands up their legs to brace themselves as they rise to a standing position.
Another classic symptom of muscular dystrophy is known as the "slip through" symptom. Your child's physician puts his/her hands around the sides of the child's chest, right up under the arms. As the child is lifted up, the shoulders weaken and move upward, almost allowing the child to slip through the physician's hands.
In addition, children with muscular dystrophy often have very large calf muscles due to the large amounts of fatty deposits that are replacing muscle.
The symptoms of muscular dystrophy may resemble other conditions or medical problems. Always consult your child's physician for a diagnosis.
How is muscular dystrophy diagnosed?
The diagnosis of muscular dystrophy is made with a physical examination and diagnostic testing by your child's physician. During the examination, your child's physician obtains a complete prenatal and birth history of the child and asks if other family members are known to have muscular dystrophy.
Diagnostic tests for muscular dystrophy may include:
 |
blood tests | |
 |
Muscle Biopsy: The removal of a small sample of muscle tissue to examined under a microscope; the primary test used to confirm the diagnosis. | |
 |
Electromyogram (EMG): Test to check if the muscle weakness is a result of destruction of muscle tissue rather than nerve damage. | |
 |
electrocardiogram (ECG or EKG): A test that records the electrical activity of the heart, shows abnormal rhythms (arrhythmias or dysrhythmias), and detects heart muscle damage. |
Treatment for Muscular Dystrophy:
Specific treatment for muscular dystrophy will be determined by your child's physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
To date, there is no known treatment, medicine, or surgery that will cure muscular dystrophy, or stop the muscles from weakening. The goal of treatment is to prevent deformity and allow the child to function as independently as possible.
Since muscular dystrophy is a life-long condition that is not correctable, management includes focusing on preventing or minimizing deformities and maximizing the child's functional ability at home and in the community.
Management of muscular dystrophy is either non-surgical or surgical. Non-surgical interventions may include:
 |
physical therapy | |
 |
positioning aids (to help the child sit, lie, or stand) | |
 |
braces and splints (to prevent deformity, promote support, or provide protection) | |
 |
medications | |
 |
nutritional counseling | |
 |
psychological counseling |
Surgical interventions may be considered to manage the following conditions:
 |
scoliosis (a sideways curvature of the back bones) associated with muscular dystrophy | |
 |
maintaining the child's ability to sit or stand |
Long-term outlook for a child with muscular dystrophy:
Muscular dystrophy is a progressive condition that needs life-long management to prevent deformity and complications. Walking and sitting often becomes more difficult as the child grows. Usually by the age of 12, the child needs a wheelchair because the leg muscles are too weak to work. Heart or lung problems often occur by the late teenage years or into the early 20s.
The interdisciplinary healthcare team will work with your family to improve your child's functional outcomes and to provide support as you learn to care for your child's needs.
The Muscular Dystrophy Association (MDA) can be an important resource, both financially and emotionally, for parents of children with muscular dystrophy.
Neurocutaneous Syndromes
What are Neurocutaneous Syndromes?
Neurocutaneous syndrome is a broad term for a group of neurologic (brain, spine, and peripheral nerve) disorders. These diseases are life-long conditions that can cause tumors to grow inside the brain, spinal cord, organs, skin, and skeletal bones.
The three most common types of neurocutaneous syndromes include the following:
 |
Tuberous sclerosis (TS) | |
 |
Neurofibromatosis (NF): Type I, Type II, and schwannomatosis | |
 |
Sturge-Weber disease |
What causes Neurocutaneous Syndromes?
Tuberous sclerosis, NF, and Sturge-Weber disease are all conditions that are congenital (present at birth).
Although the true prevalence of tuberous sclerosis is not known, it is estimated that this disease occurs in one in 6,000 persons in the US. It is an autosomal dominant condition. Autosomal means that both males and females are equally affected and dominant means that only one copy of the gene is necessary to have the disorder. Many children born with TS are the first cases in a family, since the majority of TS is caused by a new gene change (mutation), and is not inherited. However, parents of a child with TS may have very subtle symptoms of the disorder, and should be carefully examined. Even if no symptoms are present, the parents are considered at a slightly increased risk to have another child with TS, greater than that of the general population.
According to the National Institute of Neurological Disorders and Stroke (NINDS), fibromatosis Type 1 (NF1) occurs in about one in 3,000 to 4,000 births in the US. NF1 is an autosomal dominant condition caused by a gene on chromosome 17, which is inherited from a parent with the disease (in half of the cases). Neurofibromatosis Type 2 (NF2) occurs less frequently, affecting about one in 25,000 births in the US. The gene which causes NF2 is found on chromosome 22.
A parent with NF has a 50/50 chance of having a child with the disease.
NF may also be the result of a new gene change (mutation). Thirty percent to fifty percent of NF cases are caused by a new mutation and are not inherited. Males and females are equally affected, regardless of how the disease occurs. Schwannomatosis is a recently-recognized form of NF that is genetically distinct from NF1 and NF2. It occurs rarely, and only 15 percent of cases are the inherited form.
The cause of Sturge-Weber disease is unknown and is considered to be sporadic (occurs by chance). Sometimes, other family members will have hemangiomas (a benign growth that consists of blood vessels) to a lesser degree than the person with Sturge-Weber disease.
What are the symptoms of Neurocutaneous Syndromes?
The following are the most common symptoms of tuberous sclerosis, neurofibromatosis, and Sturge-Weber disease. However, each individual may experience symptoms differently. Symptoms may include:
A.Tuberous Sclerosis
Growths, called tubers, are often found growing inside of the brain and retinal area of the eye. Tuberous sclerosis affects many organs in the body including the brain, spinal cord, lungs, heart, kidneys, skin, and skeletal bones. Mental retardation, developmental delays, seizures, and learning disabilities are also associated with this disease.
B.Neurofibromatosis (NF)
There are three distinct types of NF, classified as NF I, NF II, and schwannomatosis.
| 1. | Neurofibromatosis I: This is the more common of the two disorders. It is also called Von Recklinghausen's disease. The classic symptom of NF I is light brown patches of pigment on the skin, called café-au-lait spots. Benign (non-cancerous) skin tumors associated with this condition are called neurofibromas. Neurofibromas are often found growing on the nerves and in various organs of the person's body. There is a high rate of brain tumors in patients associated with NF. Less than one percent of individuals with NF will have malignant (cancerous) changes in the neurofibromas. Lisch nodules, which are small tumors on the iris (colored part of the eye), may appear around adolescence, but usually do not cause problems. Hearing loss, headaches, seizures, scoliosis, and facial pain or numbness may also be present. Mental retardation is present in up to one percent of individuals with neurofibromatosis I, while other persons affected may have learning problems and hyperactivity. | |
| 2. | Neurofibromatosis II: According to the NINDS, this type of neurofibromatosis affects approximately one in 25,000 people, and symptoms are usually noticed between 18 and 22 years of age. It is known as bilateral acoustic neurofibromatosis and is less common. This disease is characterized by tumors on the eighth cranial nerve, which can lead to hearing loss, headaches, problems with facial movements, problems with balance, and difficulty walking. Hearing loss may be noted as early as the teenage years. Other clinical signs of NF II may include seizures, neurofibromas (skin nodules), and café-au-lait spots (although these are not nearly as common as in NF I). | |
| 3. | Schwannomatosis: The primary feature which distinguishes schwannomatosis from NF1 and NF2 is the growth of multiple schwannomas throughout the body except the vestibular nerve is not involved. Extremely intense pain is the main symptom, which occurs when a schwannoma becomes larger or presses on a nerve or nearby tissue. Other symptoms that may be experienced include numbness, tingling, or weakness in the fingers and toes. |
C.Sturge-Weber Disease
The classic symptom of this disease is a port-wine stain located on the face, typically near or around the eye and forehead areas. A port-wine stain is present from birth and is a flat area that varies in color from red to dark purple. The birthmark is caused by the formation of too many tiny blood vessels under the skin. There may also be associated brain abnormalities on the same side of the brain as the face lesion. Neurological changes that occur with this condition may include seizures, muscle weakness, changes in vision, and mental retardation. Glaucoma (a condition that causes increased pressure in the eye) may also be present at birth. Unlike tuberous sclerosis and NF, Sturge-Weber disease does not affect the other organs of the body.
The symptoms of neurocutaneous syndromes may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How are neurocutaneous syndromes diagnosed?
Tuberous sclerosis, NF, and Sturge-Weber disease are congenital (present at birth). The diagnosis is made with a physical examination and diagnostic tests. During the examination, the physician obtains a complete medical history and asks if other family members are known to have any of these conditions. In babies and children, the physician will also ask about developmental milestones, since these disorders can be associated with other neurological problems and may require further medical follow-up.
Diagnostic tests may include:
 |
Blood tests | |
 |
Genetic testing: Diagnostic tests that evaluate for conditions that have a tendency to run in families. | |
 |
X-ray: A diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. | |
 |
Magnetic Resonance Imaging (MRI): A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. | |
 |
Computed Tomography Scan (Also called a CT or CAT scan.): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
 |
Electroencephalogram (EEG): A procedure that records the brain's continuous, electrical activity by means of electrodes attached to the scalp. | |
 |
Eye examination | |
 |
Tissue sample of the tumor or skin lesion |
Treatment of neurocutaneous syndromes:
Specific treatment for neurocutaneous syndromes will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
Since neurocutaneous syndromes are life-long conditions that are not curable, the focus is on medically managing the symptoms. A person is best treated with an interdisciplinary team that may include the following healthcare providers:
 |
Pediatrician/family practitioner | |
 |
Neurologist - a physician who specializes in conditions of the brain, nerves, and spinal cord. | |
 |
Neurosurgeon - a surgeon who specializes in operating on the brain and spinal cord. | |
 |
Orthopaedic surgeon - a surgeon who specializes in conditions of the muscles, tendons, ligaments, and bone. | |
 |
Ophthalmologist - a physician who specializes in conditions of the eye. | |
 |
Nurse | |
 |
Rehabilitation team (physical, occupational, speech therapy, audiology) |
Surgery may be needed to remove tumors that may be cancerous, as well as for cosmetic reasons.
Life-long considerations for a person with Neurocutaneous Syndromes:
Since tuberous sclerosis, NF, and Sturge-Weber disease are life-long conditions that are not correctable, management includes focusing on preventing or minimizing deformities and maximizing the person's capabilities at home and in the community. Positive reinforcement will encourage the person to strengthen his/her self-esteem and promote independence.
In children, the full extent of the disease is usually not completely understood immediately after birth, but may be revealed as the child grows and develops.
Genetic counseling may be recommended by the physician to provide information on the recurrence risks for these disorders and any available testing.
Parkinson's Disease
Parkinson's Disease
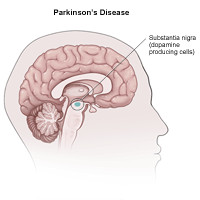
Parkinson's disease (PD or, simply, Parkinson's) is the most common form of parkinsonism, a group of motor system disorders. It is a slowly progressing, degenerative disease that is usually associated with the following symptoms, all of which result from the loss of dopamine-producing brain cells:
 |
Tremor or trembling of the arms, jaw, legs, and face | |
 |
Stiffness or rigidity of the limbs and trunk | |
 |
Bradykinesia (slowness of movement) | |
 |
Postural instability, or impaired balance and coordination |
Dopamine is a substance produced in the body which has many effects, including smooth and coordinated muscle movement.
Facts about Parkinson's Disease:
It is a myth that Parkinson's disease was cured after the introduction of levodopa (L-dopa) in the 1960s. In fact, about 60,000 Americans are newly diagnosed with Parkinson's disease each year, with more than 1 million Americans affected at any one time. Further, more people suffer from Parkinson's disease than multiple sclerosis, muscular dystrophy, and amyotrophic lateral sclerosis combined.
What causes Parkinson's Disease (PD)?
The specific cause of PD is unknown; however, medical experts believe the symptoms are related to a chemical imbalance in the brain caused by brain-cell death. Parkinson's disease is chronic (persists over a long period of time), and progressive (symptoms grow worse over time).
Although the disease may appear in younger patients (even teenagers), it usually affects people in late middle age. It is not contagious, nor is it likely passed on from generation to generation.
The biggest risk factor for developing PD is advancing age. The average age for the onset of PD is 60 years. In addition, 50 percent more men are affected than women, according to the National Institute of Neurological Disorders and Stroke. However, the reason for this is unclear.
Family history is another important risk factor. Individuals with a parent or sibling who are affected have approximately two times the chance of developing PD. This increased risk is most likely because of a combination of environmental and genetic factors.
Environmental causes are being researched and the strong consistent findings are that rural living, exposure to well water, and exposure to agricultural pesticides and herbicides are related to PD. It is important to remember, however, that these factors do not guarantee the development of PD, nor does their absence prevent it. Having one or more close relatives with PD increases one's risk of developing the disease; however, unless there is a known genetic mutation for PD present, the increased risk is only 2 percent to 5 percent.
Currently researchers believe that in most individuals the cause of PD is a combination of genetics and environmental exposure.
Parkinson's Syndrome, Atypical Parkinson's, or Parkinsonism
Parkinson's disease is also called primary parkinsonism or idiopathic Parkinson's disease. (Idiopathic is the term for a disorder for which no cause has yet been identified).
In the other forms of parkinsonism, either the cause is known or suspected, or the disorder occurs as a secondary effect of another primary neurological disorder that may have both primary and secondary symptoms of Parkinson's disease. These disorders, described as Parkinson's Syndrome, Atypical Parkinson's, or, simply, parkinsonism, may include the following:
 |
Tumors in the brain | |
 |
Repeated head trauma | |
 |
Drug-induced parkinsonism - prolonged use of tranquilizing drugs, such as the phenothiazines, butyrophenones, reserpine, and the commonly used drug, metoclopramide for stomach upset. | |
 |
Toxin-induced parkinsonism - manganese and carbon monoxide poisoning. | |
 |
Postencephalitic parkinsonism - a viral disease that causes "sleeping sickness." | |
 |
Striatonigral degeneration - the substantia nigra of the brain is only mildly affected, while other areas of the brain show more severe damage. | |
 |
Parkinsonism that accompanies other neurological conditions - such as Shy-Drager syndrome (multiple system atrophy, once thought to be a distinct disease, this is now commonly thought to be simply extensive progression of idiopathic PD), progressive supranuclear palsy, Wilson's disease, Huntington's disease, Hallervorden-Spatz syndrome, Alzheimer's disease, Creutzfeldt-Jakob disease, olivopontocerebellar atrophy, post-traumatic encephalopathy, and dementia with Lewy bodies. |
What are the four primary symptoms of Parkinson's?
The following are the most common symptoms of Parkinson's disease. However, each individual may experience symptoms differently. Symptoms may include:
 |
Muscle Rigidity: Stiffness when the arm, leg, or neck is moved back and forth. | |
 |
Resting Tremor: Tremor (involuntary movement from contracting muscles) that is most prominent at rest. | |
 |
Bradykinesia: Slowness in initiating movement. | |
 |
Postural Instability: Poor posture and balance that may cause falls; gait or balance problems. |
Other symptoms of Parkinson's disease (PD):
Symptoms of Parkinson's disease vary from patient to patient. The symptoms may appear slowly and in no particular order. Early symptoms may be subtle and may progress over many years before reaching a point where they interfere with normal daily activities.
The four cardinal symptoms of PD are listed above. Other symptoms are divided into motor (movement related) and nonmotor symptoms.
A. Motor symptoms
 |
Tremor | |
 |
Bradykinesia (slow movement) | |
 |
Rigidity and freezing in place | |
 |
Stooped posture | |
 |
Shuffling gait | |
 |
Decreased arm swing when walking | |
 |
Difficulty rising from a chair | |
 |
Micrographia (small, cramped handwriting) | |
 |
Lack of facial expression | |
 |
Slowed activities of daily living (e.g., eating, dressing, bathing, etc.) | |
 |
Difficulty turning in bed | |
 |
Remaining in a certain position for a long period of time |
B. Non-motor symptoms
 |
Diminished sense of smell | |
 |
Low voice volume (hypophonia) | |
 |
Difficulty speaking (dysarthria) | |
 |
Painful foot cramps | |
 |
Sleep disturbance | |
 |
Depression | |
 |
Emotional changes (fearful and insecure) | |
 |
Skin problems | |
 |
Constipation | |
 |
Drooling | |
 |
Increased sweating | |
 |
Urinary frequency/urgency | |
 |
Male erectile dysfunction |
As the disease progresses, walking may become affected, causing the patient to stop in mid-stride or "freeze" in place, and maybe even fall over. Patients also may begin walking with a series of quick, small steps as if hurrying forward to keep balance, a practice known as festination.
The symptoms of Parkinson's disease may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
How is Parkinson's disease diagnosed?
Making an accurate diagnosis in the early stages of Parkinson's disease can be difficult, as the beginning signs and symptoms may be considered to be indications of other conditions or the effects of normal aging. For this reason, observation of the patient may be required for some time until the symptoms are consistently present.
Currently, there are no blood or laboratory tests that are useful in the diagnosis of PD. Diagnosis of PD is based primarily on a medical history and thorough neurological examination. Brain scans and/or lab tests may be performed to help rule out other diseases or conditions, but brain scan generally will turn out to be normal with PD.
Methods to assist with the diagnosis of PD include:
 |
Neurological examination (including evaluation of symptoms and their severity) | |
 |
Trial test of drugs: When symptoms are significant, a trial test of drugs (primarily levodopa [L-dopa]) may be used to further diagnose the presence of PD. If a patient fails to benefit from levodopa, a diagnosis of Parkinson's disease may be questionable. | |
 |
Computed tomography scan (Also called a CT or CAT scan.): A diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays. | |
 |
Magnetic Resonance Imaging (MRI): A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. |
Treatment for Parkinson's Disease:
Specific treatment for a Parkinson's disease will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
With today's medicine, we have yet to find a cure for Parkinson's disease. However, based upon the severity of the symptoms and medical profile, the physician will establish an appropriate treatment protocol. Treatment for Parkinson's disease may include the following:
 |
Medications | |
 |
Surgery | |
 |
Complementary and supportive therapies, such as diet, exercise, physical therapy, occupational therapy, and speech therapy |
Medication for Parkinson's Disease:
Once the diagnosis of PD has been made, the next decision is whether a patient should receive medication, which depends on the following:
 |
The degree of functional impairment | |
 |
The degree of cognitive impairment | |
 |
Ability to tolerate antiparkinsonian medication | |
 |
The advice of the attending physician |
No two patients react the same way to a given drug, therefore, it takes time and patience to find an appropriate medication and dosage to alleviate symptoms.
Surgery for Parkinson's disease:
Based on the severity of the condition and the medical profile, the physician may recommend surgery as one treatment option for Parkinson's disease.
There are several types of surgery that may be performed that can help patients with Parkinson's disease. Most of the treatments are aimed at helping the tremor or rigidity that comes with the disease. In some patients, surgery may decrease the amount of medication that is needed to control the symptoms of Parkinson's disease, including the following:
There are three types of surgeries that may be performed for Parkinson's disease, including the following:
 |
Lesion Surgery (burning of tissue): In this procedure, deep parts of the brain are targeted and small lesions are made in critical parts of the brain that help control movement. The surgery may be done while the patient is awake to help determine the exact placement of the lesion. The lesion is placed to help control, or stop, the area of the brain that is causing the tremor. | |
 |
Deep brain stimulation (DBS): with this type of surgery, a small electrode is placed in the critical parts of the brain that help to control movement. The electrode is attached to a small battery in the chest wall and is connected by wires that are placed under the skin. The stimulator is then turned on and interrupts the normal flow of information in the brain and can help to decrease symptoms of Parkinson's disease. | |
 |
Neural grafting or tissue transplants Experimental research is being done to find a replacement for the part of the brain that functions improperly in Parkinson's disease. |
It is important to remember that surgery may help with symptoms of Parkinson's disease, but does not cure the disease or stop the progression of the disease.
Mental Health & Psychiatry
Mental health disorders strike millions people, Some disorders are mild, while others are more disabling and require intensive management and care. If left untreated, a mental health disorder can continue for months or years and may affect your personal relationships, work life and social life.
Areas of focus include anxiety and panic attacks, depression, post-traumatic disorders, family and marital conflict, personality disorders, schizophrenia, and sexual abuse
Eating Disorders
The term eating disorders refers to a variety of disorders. The common feature of all the eating disorders is abnormal eating behaviors. Eating disorders are serious mental health problems and can be life threatening. Anorexia nervosa, bulimia nervosa, and binge eating disorder are common eating disorders among adolescents and young adults. Obesity may also be included as an eating disorder and can affect individuals of all ages, including children, adolescents, and adults. There are several types of eating disorders that require the clinical care of a psychiatrist or other mental health professional
Generalized Anxiety Disorder
Anxiety disorders include panic disorder, obsessive-compulsive disorder (OCD), post-traumatic stress disorder, generalized anxiety disorder (GAD), and phobias (social phobia, agoraphobia, and specific phobia). Many anxiety disorders are accompanied by substance abuse, eating disorders, and depression. Many people experience more than one anxiety disorder at one time.
What is generalized Anxiety Disorder?
Generalized anxiety disorder (GAD) causes its sufferers chronic and exaggerated worry and tension that seem to have no substantial cause. People with generalized anxiety disorder often worry excessively about health, money, family, or work, and continually anticipate disaster. Although GAD may be accompanied by depression, substance abuse, or another anxiety disorder, impairment is usually mild, except in severe cases. Generally, people with this disorder do not:
 |
Feel too restricted in social settings. | |
 |
Feel too restricted on the job. | |
 |
Avoid certain situations. |
What are the characteristics of Generalized Anxiety Disorder?
People with this disorder usually realize that their anxiety is more intense than the situation warrants, but cannot rid themselves of these irrational concerns. The following are the most common symptoms of GAD. However, each individual may experience symptoms differently. Symptoms may include:
 |
Trouble falling or staying asleep | |
 |
Trembling | |
 |
Twitching | |
 |
Muscle tension | |
 |
Headaches | |
 |
Irritability | |
 |
Sweating | |
 |
Hot flashes | |
 |
Lightheadedness and/or difficulty breathing | |
 |
Nausea | |
 |
Frequent urination | |
 |
Feeling as though there is a lump in the throat | |
 |
Fatigue | |
 |
Lack of concentration | |
 |
Being easily startled | |
 |
Prone to irritable bowel syndrome | |
 |
Inability to relax |
The symptoms of GAD may resemble other psychiatric conditions. Always see your doctor for a diagnosis.
Who is affected by GAD?
GAD begins gradually, usually in childhood or adolescence, but can begin in adulthood, too. It is more commonly seen in women and often occurs in relatives of those affected. Each year, 3.1 percent of people ages 18 and 54 are affected by GAD, and approximately 6.8 million American adults have it.
How is generalized Anxiety disorder diagnosed?
GAD is diagnosed by a doctor or mental health professional, who can help determine whether the symptoms you are experiencing are related to an anxiety disorder or another medical condition.
Treatment for generalized anxiety disorder
Specific treatment for GAD will be determined by your doctor based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
Treatment may include:
 |
Medications | |
 |
Surgery | |
 |
Complementary and supportive therapies, such as diet, exercise, physical therapy, occupational therapy, and speech therapy |
Adjustment Disorders
What is an adjustment disorder?
An adjustment disorder is defined as an emotional or behavioral reaction to an identifiable stressful event or change in a person's life that is considered maladaptive or somehow not an expected healthy response to the event or change. The reaction must occur within three months of the identified stressful event or change happening. The identifiable stressful event or change in the life of a child or adolescent may be a family move, parental divorce or separation, the loss of a pet, birth of a brother or sister, to name a few.
What causes adjustment disorders?
Adjustment disorders are a reaction to stress. There is not a single direct cause between the stressful event and the reaction. Children and adolescents vary in their temperament, past experiences, vulnerability, and coping skills. Their developmental stage and the capacity of their support system to meet their specific needs related to the stress are factors that may contribute to their reaction to a particular stress. Stressors also vary in duration, intensity, and effect. No evidence is available to suggest a specific biological factor that causes adjustment disorders.
Who is affected by adjustment disorders?
Adjustment disorders are quite common in children and adolescents. They occur equally in males and females. While adjustment disorders occur in all cultures, the stressors and the signs may vary based on cultural influences. Adjustment disorders occur at all ages, however, it is believed that characteristics of the disorder are different in children and adolescents than they are in adults. Differences are noted in the symptoms experienced, severity and duration of symptoms, and in the outcome. Adolescent symptoms of adjustment disorders are more behavioral such as acting out, while adults experience more depressive symptoms.
What are the symptoms of an adjustment disorder?
In all adjustment disorders, the reaction to the stressor seems to be in excess of a normal reaction, or the reaction significantly interferes with social or occupational (educational) functioning. There are six subtypes of adjustment disorder that are based on the type of the major symptoms experienced. The following are the most common symptoms of each of the subtypes of adjustment disorder. However, each child may experience symptoms differently. Symptoms may include:
A. Adjustment disorder with depressed mood
 |
depressed mood | |
 |
tearfulness | |
 |
feelings of hopelessness |
B. Adjustment disorder with anxiety
 |
nervousnessd | |
 |
worry | |
 |
jitteriness | |
 |
fear of separation from major attachment figures |
C. adjustment disorder with anxiety and depressed mood A combination of symptoms from both of the above subtypes (depressed mood and anxiety) is present.
D. adjustment disorder with disturbance of conduct
 |
violation of the rights of others | |
 |
violation of societal norms and rules (truancy, destruction of property, reckless driving, fighting) |
E. adjustment disorder with mixed disturbance of emotions and conduct A combination of symptoms from all of the above subtypes are present (depressed mood, anxiety, and conduct).
F. Adjustment Disorder Unspecified: Reactions to stressful events that do not fit in one of the above subtypes are present. Reactions may include behaviors such as social withdrawal or inhibitions to normally expected activities (i.e., school or work). The symptoms of adjustment disorders may resemble other medical problems or psychiatric conditions. Always consult your child's (adolescent's) physician for a diagnosis.
How are adjustment disorders diagnosed?
A child and adolescent psychiatrist or a qualified mental health professional usually makes the diagnosis of an adjustment disorder in children and adolescents following a comprehensive psychiatric evaluation and interview with the child or adolescent and the parents. A detailed personal history of development, life events, emotions, behaviors, and the identified stressful event is obtained during the interview.
Treatment for adjustment disorders:
Specific treatment for adjustment disorders will be determined by your child's (adolescent's) physician based on:
 |
your child's (adolescent's) age, overall health, and medical history | |
 |
extent of your child's (adolescent's) symptoms | |
 |
subtype of the adjustment disorder | |
 |
your child's (adolescent's) tolerance for specific medications, procedures, or therapies | |
 |
expectations for the course of the stressful event | |
 |
your opinion or preference |
Treatment may include:
 |
individual psychotherapy using cognitive-behavioral approaches Cognitive-behavioral approaches are used to improve age-appropriate problem solving skills, communication skills, impulse control, anger management skills, and stress management skills. | |
 |
family therapy Family therapy is often focused on making needed changes within the family system such as improving communication skills and family interactions, as well as increasing family support among family members. | |
 |
peer group therapy Peer group therapy is often focused on developing and using social skills and interpersonal skills. | |
 |
medication While medications have very limited value in the treatment of adjustment disorders, medication may be considered on a short term basis if a specific symptom is severe and known to be responsive to medication. |
Prevention of adjustment Disorders
Preventive measures to reduce the incidence of adjustment disorders in children are not known at this time. However, early detection and intervention can reduce the severity of symptoms, enhance the child's normal growth and development, and improve the quality of life experienced by children or adolescents with adjustment disorders.
Behavior Disorders
Did You Know?
Boys are two to three times more likely to have ADHD than girls.
Behavior disorders (sometimes referred to as disruptive behavior disorders) are the most common reasons children are referred for mental health evaluations and treatment. All disruptive behavior is not the same. Behavior disorders include mental health problems with a focus on behaviors that both identify emotional problems and create interpersonal and social problems for children and adolescents in the course of their development.
The most common behavior disorder in children is attention-deficit/hyperactivity disorder (ADHD). Conduct disorder focuses on the mental health problems identified and created by more disruptive behaviors. Oppositional defiant disorder is yet another behavior disorder that focuses on the behavior that is disruptive to relationships with others.
There are many types of behavioral disorders that require clinical care by a physician or other healthcare professional
Mood Disorders
While major depressive disorder can develop at any age, the average age at onset is the mid-20s.
The average age of onset for a first manic episode of bipolar disorder is during the early 20s.
What are Mood Disorders?
Mood disorders refer to a category of mental health problems that include all types of depression and bipolar disorder. Mood disorders are sometimes called affective disorders.
What causes Mood Disorders?
What causes mood disorders is not well known. There are chemicals in the brain, called endorphins, that are responsible for positive moods. Other chemicals in the brain, called neurotransmitters, regulate endorphins. Most likely, depression (and other mood disorders) is caused by a chemical imbalance in the brain. Life events (such as unwanted changes in life) may also contribute to a depressed mood.
Affective disorders aggregate in families and are considered to be multifactorially inherited. Multifactorial inheritance means that "many factors" are involved. The factors that produce the trait or condition are usually both genetic and environmental, involving a combination of genes from both parents. Often one gender (either males or females) is affected more frequently than the other in multifactorial traits. There appears to be a different threshold of expression, which means that one gender is more likely to show the problem, over the other gender.
Who is affected by Mood Disorders?
Anyone can feel sad or depressed at times. However, mood disorders are more intense and difficult to manage than normal feelings of sadness. Children, adolescents, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder. However, life events and stress can expose or exaggerate feelings of sadness or depression, making the feelings more difficult to manage. Sometimes, life's problems can trigger depression. Being fired from a job, getting divorced, losing a loved one, death in the family, and financial trouble, to name a few, all can be difficult and coping with the pressure may be troublesome. These life events and stress can bring on feelings of sadness or depression or make a mood disorder harder to manage. The chance for depression in females in the general population is nearly twice as high (12 percent) as it is for males (6.6 percent). Once a person in the family has this diagnosis, the chance for their siblings or children to have the same diagnosis is increased. In addition, relatives of persons with depression are also at increased risk for bipolar disorder (manic depression). The chance for manic depression (or bipolar disorder) in males and females in the general population is about 2.6 percent. Once a person in the family has this diagnosis, the chance for their siblings or children to have the same diagnosis is increased. In addition, relatives of persons with manic depression are also at increased risk for depression.
What are the symptoms of Mood Disorders?
Depending upon age and the type of mood disorder present, a person may exhibit different symptoms of depression. The following are the most common symptoms of a mood disorder. However, each individual may experience symptoms differently. Symptoms may include:
 |
persistent feelings of sadness | |
 |
feeling hopeless or helpless | |
 |
having low self-esteem | |
 |
feeling inadequate | |
 |
excessive guilt | |
 |
feelings of wanting to die | |
 |
loss of interest in usual activities or activities once enjoyed | |
 |
difficulty with relationships | |
 |
sleep disturbances (i.e., insomnia, hypersomnia) | |
 |
changes in appetite or weight | |
 |
decreased energy | |
 |
difficulty concentrating | |
 |
a decrease in the ability to make decisions | |
 |
suicidal thoughts or attempts | |
 |
frequent physical complaints (i.e., headache, stomach ache, fatigue) | |
 |
running away or threats of running away from home | |
 |
hypersensitivity to failure or rejection | |
 |
irritability, hostility, aggression |
In mood disorders, these feelings appear more intense than what a person may normally feel from time to time. It is also of concern if these feelings continue over a period of time, or interfere with an individual's interest in family, friends, community, or work. Any person who expresses thoughts of suicide should be evaluated immediately.
The symptoms of mood disorders may resemble other conditions or psychiatric problems. Always consult your physician for a diagnosis.
How are mood disorders diagnosed?
Mood disorders are a real medical disorder. A psychiatrist or other mental health professional usually diagnoses mood disorders following a comprehensive psychiatric evaluation.
Treatment for mood disorders:
Specific treatment for mood disorders will be determined by your physician based on:
 |
your child's (adolescent's) age, overall health, and medical history | |
 |
extent of your child's (adolescent's) symptoms | |
 |
subtype of the adjustment disorder | |
 |
your child's (adolescent's) tolerance for specific medications, procedures, or therapies | |
 |
expectations for the course of the stressful event | |
 |
your opinion or preference |
Mood disorders can often be effectively treated. Treatment should always be based on a comprehensive evaluation. Treatment may include one, or more, of the following:
 |
antidepressant medications (especially when combined with psychotherapy has shown to be very effective in the treatment of depression) | |
 |
psychotherapy (most often cognitive-behavioral and/or interpersonal therapy that is focused on changing the individual's distorted views of themselves and the environment around them, working through difficult relationships, and identifying stressors in the environment and how to avoid them) | |
 |
family therapy |
Families play a vital supportive role in any treatment process.
Prevention of Mood Disorders:
Preventive measures to reduce the incidence of mood disorders are not known at this time. However, early detection and intervention can reduce the severity of symptoms, enhance the individual's normal growth and development, and improve the quality of life experienced by persons with mood disorders.
Manic Depression / Bipolar Disorder
What is Manic Depression?
Manic depression, also known as bipolar disorder, is classified as a type of affective disorder or mood disorder that goes beyond the day's ordinary ups and downs, and is a serious medical condition and important health concern in this country. Manic depression is characterized by periodic episodes of extreme elation, elevated mood, or irritability (also called mania) countered by periodic, classic depressive symptoms.
Depression is a mood disorder that involves a child's body, mood, and thoughts. It can affect and disrupt eating, sleeping, or thinking patterns, and is not the same as being unhappy or in a "blue" mood, nor is it a sign of personal weakness or a condition that can be willed or wished away. Children with a depressive illness cannot merely "pull themselves together" and get better. Treatment is often necessary and many times crucial to recovery.
There are three primary types of depression, including:
 |
major depression (clinical depression) | |
 |
bipolar disorder (manic depression) | |
 |
dysthymic disorder (dysthymia) |
Who is affected by Manic Depression?
Manic depression affects more than 5.7 million American adults - or about 2.6 percent of Americans age 18 and older in a given year. When symptoms are present before the age of 12, they are often confused with attention-deficit/hyperactivity disorder (ADHD) - a syndrome that is usually characterized by serious and persistent difficulties resulting in inattentiveness or distractibility, impulsivity, and hyperactivity.
Affecting men and women equally (although women are more likely to experience more depressive and less manic symptoms), manic depression often begins in adolescence or early adulthood. In fact, the median age of onset is 25.
Manic depression is likely to run in families and, in some cases, is believed to be hereditary. Researchers are still undergoing intense research to identify a gene that may be responsible for this disorder.
What are the symptoms of manic depression?
The following are the most common symptoms of manic depression. However, each individual may experience symptoms differently.
Depressive symptoms may include:
 |
persistent sad, anxious, or empty mood | |
 |
loss of interest in activities once previously enjoyed | |
 |
excessive crying | |
 |
increased restlessness and irritability | |
 |
decreased ability to concentrate and make decisions | |
 |
decreased energy | |
 |
thoughts of death or suicide, or suicide attempts | |
 |
increased feelings of guilt, helplessness, and/or hopelessness | |
 |
weight and/or appetite changes due to over- or under-eating | |
 |
changes in sleep patterns | |
 |
social withdrawal | |
 |
physical symptoms unrealized by standard treatment (i.e., chronic pain, headaches) |
Manic symptoms may include:
 |
overly inflated self-esteem | |
 |
decreased need for rest and sleep | |
 |
increased distractibility and irritability | |
 |
increased physical agitation | |
 |
excessive involvement in pleasurable activities that may result in painful consequence; this may include provocative, aggressive, or destructive behavior | |
 |
increased talkativeness | |
 |
excessive "high" or euphoric feelings | |
 |
increased sex drive | |
 |
increased energy level | |
 |
uncharacteristically poor judgment | |
 |
increased denial |
For a diagnosis of manic depression to be made, an individual must exhibit both depressive and manic symptoms to a varying degree, depending upon the severity of the disorder. The symptoms of manic depression may resemble other psychiatric conditions. Always consult your physician for a diagnosis.
How is manic depression diagnosed?
Because depression has shown to often co-exist with other medical conditions, such as heart disease, cancer, or diabetes, and other psychiatric disorders, such as substance abuse, or anxiety disorders, seeking early diagnosis and treatment is crucial to recovery. A diagnosis is often made after a careful psychiatric examination and medical history performed by a psychiatrist or other mental health professional.
Treatment for Manic Depression
Specific treatment for manic depression will be determined by your physician based on:
 |
your child's (adolescent's) age, overall health, and medical history | |
 |
extent of your child's (adolescent's) symptoms | |
 |
subtype of the adjustment disorder | |
 |
your child's (adolescent's) tolerance for specific medications, procedures, or therapies | |
 |
expectations for the course of the stressful event | |
 |
your opinion or preference |
Treatment may include either, or a combination, of the following:
 |
medication (i.e., mood-stabilizing anticonvulsants such as lithium, valproate, or carbamazepine, and/or antidepressants such as Prozac, Zoloft, or Paxil) | |
 |
psychotherapy (most often cognitive-behavioral and/or interpersonal therapy that is focused on changing the individual's distorted views of themselves and the environment around them, working through difficult relationships, and identifying stressors in the environment and how to avoid them) | |
 |
electroconvulsive therapy (ECT) |
Recognizing the varied and extreme mood swings associated with manic depression is crucial in obtaining effective treatment, and avoiding the potentially painful consequences of the reckless, manic behavior.
In most cases, long-term, preventive treatment is necessary to stabilize the mood swings associated with manic depression.
Personality Disorders
What are Personality Disorders?
For persons without a personality disorder, personality traits are patterns of thinking, reacting, and behaving that remain relatively consistent and stable over time. Persons with a personality disorder display more rigid and maladaptive thinking and reacting behaviors that often disrupt their personal, professional, and social lives.
What are the most common types of Personality Disorders?
Generally, personality disorders are divided into three subtypes (or clusters), and include the following:
| Specific Phobia | Classification |
| Cluster A: | odd/eccentric |
| Cluster B: | dramatic/erratic |
| Cluster C: | anxious/inhibited |
Examples of odd/eccentric (Cluster A) personality disorders:
| 1. | Paranoid Personality Disorder: Persons with this disorder are often cold, distant, and unable to form close, interpersonal relationships. Often overly, yet unjustifiably, suspicious of their surroundings, persons with paranoid personality disorder generally cannot see their role in conflict situations and often project their feelings of paranoia as anger onto others. | |
| 2. | Schizoid Personality Disorder: Persons with this disorder are often cold, distant, introverted, and have an intense fear of intimacy and closeness. Persons with schizoid personality disorder are often too absorbed in their own thinking and daydreaming that they exclude themselves from attachment with persons and reality. | |
| 3. | Schizotypal Personality Disorder: Similar to schizoid personality disorder, persons with this disorder are often cold, distant, introverted, and have an intense fear of intimacy and closeness. Yet, with schizotypal personality disorder, persons also exhibit disordered thinking, perception, and ineffective communication skills. Many symptoms of schizotypal personality disorder resemble schizophrenia, but are less mild and intrusive. |
Examples of dramatic/erratic (Cluster B) personality disorders:
| 1. | Borderline Personality Disorder: Persons with this disorder present instability in their perceptions of themselves, and have difficulty maintaining stable relationships. Moods may also be inconsistent, but never neutral - their sense of reality is always seen in "black and white." Persons with borderline personality disorder often feel as though they lacked a certain level of nurturing while growing up and, as a result, incessantly seek a higher level of caretaking from others as adults. This may be achieved through manipulation of others, leaving them often feeling empty, angry, and abandoned, which may lead to desperate and impulsive behavior. | |
| 2. | Antisocial Personality Disorder: Persons with this disorder characteristically disregard the feelings, property, authority, and respect of others, for their own personal gain. This may include violent or aggressive acts involving or targeting other individuals, without a sense or remorse or guilt for any of their destructive actions. | |
| 3. | Narcissistic Personality Disorder: Persons with this disorder present severely overly-inflated feelings of self-worth, grandiosity, and superiority over others. Persons with narcissistic personality disorder often exploit others who fail to admire them, and are overly sensitive to criticism, judgment, and defeat. | |
| 4. | histrionic personality disorder: Persons with this disorder are overly conscious of their appearance, are constantly seeking attention, and often behave dramatically in situations that do not warrant this type of reaction. The emotional expressions of persons with histrionic personality disorder are often judged as superficial and exaggerated. |
Examples of anxious/inhibited (Cluster C) personality disorders:
| 1. | Dependent Personality Disorder: Persons with this disorder rely heavily on others for validation and fulfillment of basic needs. Often unable to properly care for themselves, persons with dependent personality disorder lack self confidence and security, and are deficient in making decisions. | |
| 2. | Avoidant Personality Disorder: Persons with this disorder are hypersensitive to rejection and thus, avoid situations with any potential for conflict. This reaction is fear-driven, however, persons with avoidant personality disorder become disturbed by their own social isolation, withdrawal, and inability to form close, interpersonal relationships. | |
| 3. | Obsessive-Compulsive Personality Disorder: Persons with this disorder are inflexible to change and bothered by a disrupted routine due to their obsession for order. Thus, they experience anxiety and have trouble completing tasks and making decisions. Persons with obsessive-compulsive personality disorder often become uncomfortable in situations that are beyond their control and have difficulty maintaining positive, healthy interpersonal relationships as a result. |
Treatment for Personality Disorders:
Specific treatment for each personality disorder will be determined by your physician based on:
 |
your child's (adolescent's) age, overall health, and medical history | |
 |
extent of your child's (adolescent's) symptoms | |
 |
subtype of the adjustment disorder | |
 |
your child's (adolescent's) tolerance for specific medications, procedures, or therapies | |
 |
expectations for the course of the stressful event | |
 |
your opinion or preference |
Personality disorders are often difficult to treat and may require long-term attention to change the inappropriate behavior and thought patterns. Treatment may include:
 |
medication (although medication may be abused and has limited effectiveness) | |
 |
psychological treatment (including family involvement) |
Phobias
What is a Phobia?
According to the American Psychiatric Association, a phobia is an uncontrollable, irrational, and persistent fear of a specific object, situation, or activity. The fear experienced by people with phobias can be so great that some individuals go to extreme lengths to avoid the source of their fear. One extreme response to the source of a phobia can be a panic attack.
Who is affected by Phobias?
Every year, approximately 19 million of Americans experience one or more phobias that range from mild to severe. Phobias can occur in early childhood, but usually are first evident between the ages of 15 and 20 years. They affect both genders equally, although men are more likely to seek treatment for phobias.
What causes Phobias?
Research suggests that both genetic and environmental factors contribute to the onset of phobias. Specific phobias have been associated with a fearful first encounter with the phobic object or situation. The question still exists, however, whether this conditioning exposure is necessary or if phobias can develop in genetically predisposed individuals.
What are the three primary types of Phobias?
| Specific Phobia | What is specific phobia? Specific phobia is characterized by extreme fear of an object or situation that is not harmful under general conditions. Examples may include a fear of the following:
|
||||||||||||||||||||||||
| Specific Phobia | What is social phobia?
Social phobia is an anxiety disorder in which a person has significant anxiety and discomfort related to a fear of being embarrassed, humiliated, or scorned by others in social or performance situations. Even when they manage to confront this fear, persons with social phobia usually:
Most people experiencing social phobia will try to avoid situations that provoke dread or otherwise cause them much distress. Diagnosing social phobia: Social phobia is diagnosed when the fear or avoidance significantly interferes with normal, expected routines, or is excessively upsetting. Social phobia disrupts normal life, interfering with career or social relationships. It often runs in families and may be accompanied by depression or alcoholism. Social phobia often begins around early adolescence or even younger. Approximately 15 million American adults ages 18 to 54 experience social phobia in a given year. Treatment for social phobia: People who suffer from social phobia often find relief from their symptoms when treated with cognitive-behavioral therapy, or medications, or a combination of the two. |
||||||||||||||||||||||||
| Agoraphobia | What is agoraphobia? Agoraphobia is a Greek word that literally means "fear of the marketplace." This anxiety disorder involves the fear of experiencing a panic attack in a place or situation from which escape may be difficult or embarrassing. The anxiety associated with agoraphobia is so severe that panic attacks are not unusual, and individuals with agoraphobia typically try to avoid the location or cause of their fear. Agoraphobia involves fear of situations such as, but is not limited to, the following:
What are the characteristics of agoraphobia? Most people with agoraphobia develop the disorder after first suffering a series of one or more panic attacks. The attacks occur randomly and without warning, and make it impossible for a person to predict what situations will trigger the reaction. This unpredictability of the panic causes the person to anticipate future panic attacks and, eventually, fear any situation in which an attack may occur. As a result, they avoid going into any place or situation where previous panic attacks have occurred. People with the disorder often become so disabled that they literally feel they cannot leave their homes. Others who have agoraphobia, do go into potentially "phobic" situations, but only with great distress, or when accompanied by a trusted friend or family member. Persons with agoraphobia may also develop depression, fatigue, tension, alcohol or drug abuse problems, and obsessive disorders, making seeking treatment crucial. Approximately 1.8 million American adults ages 18 to 54 experience agoraphobia in a given year. |
Schizophrenia
What is Schizophrenia?
Schizophrenia is one of the most complex of all mental health disorders. It involves a severe, chronic, and disabling disturbance of the brain. And, what was once classified as a psychological disease is now classified as a brain disease.
What causes Schizophrenia?
There is no known single cause responsible for schizophrenia. It is believed that a chemical imbalance in the brain is an inherited factor which is necessary for schizophrenia to develop. However, it is likely that many factors--genetic, behavioral, and environmental--play a role in the development of this mental health condition.
Schizophrenia is considered to be multifactorially inherited. Multifactorial inheritance means that "many factors" are involved. The factors are usually both genetic and environmental, where a combination of genes from both parents, in addition to unknown environmental factors, produce the trait or condition. Often, one gender (either males or females) is affected more frequently than the other in multifactorial traits. There appears to be a different threshold of expression, which means that one gender is more likely to show the problem, over the other gender. Slightly more males develop schizophrenia in childhood, however, by adolescence schizophrenia affects males and females equally.
Who is affected by Schizophrenia?
Although schizophrenia affects men and women equally, symptoms in men generally begin earlier than in women. In most cases, schizophrenia first appears in men during their late teens or early 20s. In women, schizophrenia often first appears during their 20s or early 30s.
Statistics indicate that schizophrenia affects 2.7 million Americans. A child born into a family with one or more schizophrenic family member has a greater chance of developing schizophrenia than a child born into a family with no history of schizophrenia.
After a person has been diagnosed with schizophrenia in a family, the chance for a sibling to also be diagnosed with schizophrenia is 7 to 8 percent. If a parent has schizophrenia, the chance for a child to have the disorder is 10 to 15 percent. Risks increase with multiple affected family members.
What are the symptoms of Schizophrenia?
One of the most disturbing and puzzling characteristics of schizophrenia is the sudden onset of its psychotic symptoms. The following are the most common symptoms of schizophrenia. However, each individual may experience symptoms differently. Symptoms may include
 |
Distorted perception of reality (i.e., difficulty telling dreams from reality) | |
 |
Confused thinking (i.e., confusing television with reality) | |
 |
Detailed and bizarre thoughts and ideas | |
 |
Suspiciousness and/or paranoia (fearfulness that someone, or something, is going to harm them) | |
 |
Hallucinations (seeing, hearing, or feeling things that are not real such as hearing voices telling them to do something) | |
 |
Delusions (ideas that seem real but are not based in reality) | |
 |
Extreme moodiness | |
 |
Severe anxiety and/or fearfulness | |
 |
Flat affect (lack of emotional expression when speaking) or inability to manage emotions | |
 |
Difficulty in performing functions at work and/or school | |
 |
Exaggerated self-worth and/or unrealistic sense of superiority of one's self | |
 |
Social withdrawal (severe problems in making and keeping friends ) | |
 |
Disorganized or catatonic behavior (suddenly becoming agitated and confused, or sitting and staring, as if immobilized) | |
 |
Odd behaviors |
The symptoms of schizophrenia are often classified as positive (symptoms including delusions, hallucinations, and bizarre behavior), negative (symptoms including flat affect, withdrawal, and emotional unresponsiveness), disorganized speech (including speech that is incomprehensible), and disorganized or catatonic behavior (including marked mood swings, sudden aggressive, or confusion, followed by sudden motionlessness and staring).
The symptoms of schizophrenia in children are similar to adults, however, children, more often (in 80 percent of diagnosed cases), experience auditory hallucinations and typically do not experience delusions or formal thought disorders until mid-adolescence or older.
The symptoms of schizophrenia may resemble other problems or psychiatric conditions. Always consult your physician for a diagnosis.
How is schizophrenia diagnosed?
Schizophrenia is usually diagnosed by a psychiatrist. Other mental health professionals usually participate in the completion of a comprehensive mental health evaluation to determine individualized treatment needs.
Treatment for schizophrenia:
Specific treatment for schizophrenia will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the disease | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the disease | |
 |
Your opinion or preference |
Schizophrenia is a major psychiatric illness. Treatment for schizophrenia is complex. A combination of therapies is often necessary to meet the individualized needs of the individual with schizophrenia. Treatment is aimed at reducing the symptoms associated with the disorder. Types of treatment that may be helpful to an individual with schizophrenia may include:
A. Medications (also called psychopharmacological management; to reduce the symptoms of schizophrenia), including the following:
 |
Neuroleptics--a specialized class of medications used to treat schizophrenia. Neuroleptics are used primarily to treat the pervasive, intrusive, and disturbing thoughts of a person with schizophrenia. They are designed to help minimize the severity of delusions and hallucinations the individual is experiencing. | |
 |
Antipsychotic medications--medications that act against the symptoms of psychotic illness, but do not cure the illness. However, these medications can reduce symptoms or reduce the severity of symptoms; a specialized class of medications used to treat schizophrenia. |
B. Individual and family psychotherapy (including cognitive and behavioral therapy)
C. Specialized educational and/or structured activity programs (i.e., social skills training, vocational training, speech and language therapy)
D. Self-help and support groups
Prevention of Schizophrenia
Preventive measures to reduce the incidence of schizophrenia are not known at this time. However, identification and early intervention can improve the quality of life experienced by persons with schizophrenia. Further, treatment is most successful when symptoms of the first psychotic episode are addressed properly and promptly. It is crucial for an individual who is prescribed medications for the treatment of schizophrenia to remain compliant. Dosages and types of medications may need to be adjusted periodically to maintain effectiveness. Always consult your physician for more information.
Insomnia
What is Insomnia?
If you experience difficulty falling asleep, staying asleep, or enjoying a restful night's sleep, you may be suffering from insomnia. Insomnia is defined as the perception or complaint of inadequate or poor-quality sleep because of one or more of the following:
 |
difficulty falling asleep | |
 |
waking up frequently during the night with difficulty returning to sleep | |
 |
waking up too early in the morning | |
 |
non-refreshing sleep |
Insomnia is a common symptom in the US. The Institute of Medicine estimates that between 50 and 70 million Americans have chronic sleep problems.
Insomnia is classified as:
 |
transient (short term) - lasting from a single night to a few weeks | |
 |
intermittent (on and off) - episodes occur from time to time | |
 |
chronic (constant) - occurs on most nights and lasts a month or more |
What causes insomnia?
Insomnia may be caused by many factors, including the following:
 |
stress | |
 |
depression | |
 |
anxiety | |
 |
physical illness | |
 |
caffeine intake | |
 |
irregular schedules | |
 |
circadian rhythm disorders | |
 |
drugs (including alcohol and nicotine) | |
 |
occasional or chronic pain |
What are the Symptoms of Insomnia?
 |
daytime sleepiness | |
 |
low energy or fatigue | |
 |
anxiety or frustration about sleep | |
 |
attention, concentration or memory problems | |
 |
waking up tired or in pain |
Guidelines that may help sleep problems:
 |
Get up about the same time every day. | |
 |
Go to bed only when you are sleepy and get out of bed when you are awake. | |
 |
Establish pre-sleep rituals, such as a warm bath, a light bedtime snack, brushing teeth, putting on bedtime clothing or 10 minutes of reading. | |
 |
Exercise regularly. If you exercise vigorously, do this at least 3 to 6 hours before bedtime. Mild exercise - such as simple stretching or walking - should not be done closer to bedtime than 4 hours. | |
 |
Maintain a regular schedule. Regular times for meals, taking medications, doing chores, and other activities help keep your "inner clock" running smoothly. | |
 |
Avoid anything containing caffeine within 6 hours of bedtime. | |
 |
Avoid alcohol within several hours of bedtime or when you are sleepy. | |
 |
Avoid smoking close to bedtime because nicotine is a stimulant. | |
 |
Avoid falling asleep in front of the television. | |
 |
If you take naps, try to do so at the same time every day. For most people, a short mid-afternoon nap is most helpful. | |
 |
Avoid sleeping pills or use them conservatively. Most physicians avoid prescribing sleeping pills for a period of longer than 3 weeks. Never drink alcohol while taking sleeping pills. | |
 |
Reduce evening light exposure by turning off bright lights. This may help cue the body and mind for sleep. | |
 |
Expose yourself to light (through windows or a timed lamp) 30 minutes before waking to prepare for getting out of bed. | |
 |
Make your bedroom cool, dark, and quiet. If possible, remove non-sleep related items such as televisions or computers so that the room is associated only with sleep. |
People who suffer from insomnia that lasts for more than a few days should consult a physician so that the underlying cause can be identified, if possible, then treated. If you have loud, irregular snoring, jerking legs, or pauses in breathing in addition to other symptoms of insomnia, seek the advice of a physician. These symptoms may be related to sleep apnea, a potentially life-threatening condition. There are a variety of effective treatment options available
Substance Abuse / Chemical Dependency
Addiction of Alcohol and/or Drugs
Parental and peer substance use are considered two of the more common factors contributing to youthful decisions regarding substance use. The age at which adolescents begin to use alcohol is decreasing, with 25 percent of young people beginning to drink before the age of 13, according to the CDC.
Some adolescents are more at risk of developing substance-related disorders. This includes adolescents with one or more of the following conditions present: children of substance abusers; adolescents who are victims of physical, sexual, or psychological abuse; adolescents with mental health problems, especially depressed and suicidal teens; and physically disabled adolescents.
Adolescent substance abuse is believed by some to be the most commonly missed pediatric diagnosis. Adolescents who use drugs are most likely to visit a physician's office with no obvious physical findings.
Substance abuse problems are more likely to be discovered by physicians when adolescents are injured in accidents occurring while under the influence, or when they are brought for medical services because of intentional efforts to hurt themselves.
What is Substance Abuse/Chemical Dependence?
There are three different terms used to define substance-related disorders, including the following:
 |
Substance Abuse: Substance abuse is used to describe a pattern of substance (drug) use leading to significant problems or distress such as failure to attend work/school, substance use in dangerous situations (driving a car), substance-related legal problems, or continued substance use that interferes with friendships and/or family relationships. Substance abuse, as a disorder, refers to the abuse of illegal substances or the abusive use of legal substances. Alcohol is the most common legal drug of abuse. | |
 |
Substance Dependence: Substance dependence is used to describe continued use of drugs or alcohol, even when significant problems related to their use have developed. Signs include an increased tolerance or need for increased amounts of substance to attain the desired effect, withdrawal symptoms with decreased use, unsuccessful efforts to decrease use, increased time spent in activities to obtain substances, withdrawal from social and recreational activities, and continued use of substance even with awareness of physical or psychological problems encountered by the extent of substance use. | |
 |
Chemical Dependence: Chemical dependence is also used to describe the compulsive use of chemicals (drugs or alcohol) and the inability to stop using them despite all the problems caused by their use. |
What substances are most often abused?
Substances frequently abused include, but are not limited to, the following:
 |
Alcohol | |
 |
Marijuana | |
 |
Hallucinogens | |
 |
Cocaine | |
 |
Amphetamines | |
 |
Opiates | |
 |
Anabolic steroids | |
 |
Inhalants | |
 |
Methamphetamine | |
 |
Tobacco |
What causes substance Abuse/Chemical Dependence?
Cultural and societal norms influence acceptable standards of substance use. Public laws determine the legal use of substances. The question of whether there is a normative pattern of substance use remains controversial. Substance-related disorders are caused by multiple factors including genetic vulnerability, environmental stressors, social pressures, individual personality characteristics, and psychiatric problems. However, which of these factors are primary and which are secondary has not been determined in all cases.
What are the symptoms of substance Abuse/Chemical dependence?
Substance Abuse Prevention Programs for Teens There are approaches frequently used to prevent adolescent substance use and abuse, including school-based prevention programs that usually provide drug and alcohol education and interpersonal and behavior skills training. Community-based prevention programs usually involve the media and are aimed for parents and community groups. Family-focused prevention programs involve parent training, family skills training, children's social skills training, and family self-help groups. Research literature available suggests that components of family-focused prevention programs have decreased the use of alcohol and drugs in older children and improved the effectiveness of parenting skills. The following are the most common behaviors that indicate an individual is having a problem with substance abuse. However, each individual may experience symptoms differently. Symptoms may include:
 |
Getting high on drugs or getting intoxicated (drunk) on a regular basis | |
 |
Lying, especially about how much they are using or drinking | |
 |
Avoiding friends and family members | |
 |
Giving up activities they used to enjoy such as sports or spending time with non-using friends | |
 |
Talking a lot about using drugs or alcohol | |
 |
Believing they need to use or drink in order to have fun | |
 |
Pressuring others to use or drink | |
 |
Getting in trouble with the law | |
 |
Taking risks, such as sexual risks or driving under the influence of a substance | |
 |
Work performance suffers due to substance abuse before, after, or during working or business hours | |
 |
Missing work due to substance use | |
 |
Depressed, hopeless, or suicidal feelings |
The symptoms of substance abuse may resemble other medical problems or psychiatric conditions. Always consult your physician for a diagnosis.
How is Substance Abuse/Chemical Dependence Diagnosed?
A family physician, psychiatrist, or qualified mental health professional usually diagnoses substance abuse. Clinical findings often depend on the substance abused, the frequency of use, and the length of time since last used, and may include the following:
 |
Weight loss | |
 |
Constant fatigue | |
 |
Red eyes | |
 |
Little concern for hygiene |
Treatment for Substance Abuse/Chemical Dependence
Specific treatment for substance abuse/chemical dependence will be determined by your physician based on:
 |
Your age, overall health, and medical history | |
 |
Extent of the symptoms | |
 |
Extent of the dependence | |
 |
Type of substance abused | |
 |
Your tolerance for specific medications, procedures, or therapies | |
 |
Expectations for the course of the condition | |
 |
Your opinion or preference |
A variety of treatment programs for substance abuse are available on an inpatient or outpatient basis. Programs considered are usually based on the type of substance abused. Detoxification (if needed, based on the substance abused) and long-term follow-up management are important features of successful treatment. Long-term follow-up management usually includes formalized group meetings and developmentally age-appropriate psychosocial support systems, as well as continued medical supervision. Individual and family psychotherapy are often recommended to address the developmental, psychosocial, and family issues that may have contributed to and resulted from the development of a substance abuse disorder.
Calming The Nervous System With Ayurveda

Dosha (Cause) Concerns
The nervous system is governed by the vata dosha according to Ayurveda. Doshas are the bioenergetic systems of the body and vata is one of three doshas which make up the human system: vata controls movement, pitta provides metabolism, and kapha governs tissue, bones and lubrication.
Of course, it is actually not that compartmentalized because all the doshas are interdependent and interact with each other. When you eat, vata moves the food to the digestive system, lubricated by kapha, where pitta will do the digestion.
Vata is considered the most important dosha because it is identified with prana energy. According to Wikipedia, prana is the sanskrit word for “vital life” the life giving vital force that supports us all. Vata governs the mind, nervous system, psychological processes, blood circulation, the somatic nervous system, and the movement of food and wastes.
Because vata not only regulates the nervous system but also our creativity, a vata imbalance negatively affects our ability to create. There are many signs of vata imbalance; one of the most important ones for highly sensitive people is anxiety. When we become anxious, the focus of our attention shifts to the cause of our anxiety. We are then unable to move forward into our creativity until the source of our anxiety is resolved. If it remains unresolved, chronic debilitating stress is the result and we can feel blocked.
Although the vata dosha is all about movement, one important cause of anxiety is too much movement or chaos in our environment. Vata needs a balance between stability and movement to be effective. Providing vata with stability helps an individual reduce and let go of anxiety, opening the door to more creative intention. The first law of nature is survival, so safety is always the first priority. Without a feeling of safety, vata becomes bogged down; with a feeling of safety vata feels good and can flourish.
Herbs that Can Reduce Stress, Anxiety, & Tension
Bacopa Moneri is an outstanding nervine tonic used for many neurological disorders.
Evolvulus alsinoides Linn has been employed clinically for centuries for itsmemory potentiating, anxiolytic and tranquilizing properties.
Nardostachys jatamansi have neuroprotective,anti convulsant activity best antioxidant action.
Tino cordifolia is well known medhya rasayan from Ayurved
Rasaraj ras which is beneficial in paralysis, Extremely beneficial in facial paralysis, in various types of nervous disorders.
Tapyadi loha -a combination used in haemarregic condition in brain.
Ayurvedic Suppliment :: NurayuRich
Herbs have used for thousands of years in Ayurvedic medicine, Traditional Chinese Medicine and in herbalism. Herbs have been known to treat a variety of symptoms and diseases. Stress is the number one most serious health problem Herbs can be categorized in three types adaptogen, tonic, and nervine herbs. Adaptogenic herbs help the body adapt to stress through balancing the nervous system. Tonic herbs strengthen the organs and bodies system to prepare for stress. Tonic nerves are able to increase or decrease the activity of the bodily processes in a specific system.Nervine herbs heal the damage caused by stress and combat further stressful influence. Nervine herbs can be distinguished as a sedative to relax and calm the nerves or as a stimulant to perk up energy. Most herbs fit into more than one category or type of herb giving it increased ability to relieve, reduce and alleviate symptoms, illnesses and disease. Due to the fact that herbs generally correlate to specific areas or systems of the body, there are a large number of herbs that can relieve stress and anxiety. Here you can find a few of these herbs and how they affect the body.
ADAPTOGEN:
 |
Ginseng: There are several kinds of ginseng however three can be helpful at reducing stress, Siberian, Korean or Panax and Indian or Ashwagandha ginseng are all good at normalizing the body in times of stress. Ginseng is an adaptogen and a tonic, which protects the body against stress. Ginseng regulates the circulatory and immune systems, which help to support the body in times of stress. Ginseng is a popular herbal supplement for athletes because it improves performance, increases stamina, improves recovery time and boosts ones immunity. | |
 |
Maitake: Maitake is a mushroom that grows in clusters at the base of trees. It has been used in Chinese medicine as an adaptogen to enhance the immune system. Research has also indicated that it can be used to regulate blood pressure, glucose, insulin, and both serum and liver lipids, such as cholesterol, triglycerides, and phospholipids, and may also be useful for weight loss. | |
 |
Gotu Kola: Gotu Kola has a triple effect as an adaptogen, tonic and nervine herb. Gotu Kola rejuvenates the skin by stimulating repair, growth and strengthening. It also helps with stress coping and reducing anxiety. Gotu Kola improves concentration and memory. | |
 |
Wild Yam: The Wild Yam is an adaptogen and nervine, which targets the muscles and skeletal system. It acts as a muscle relaxer to reduce inflammation. It also is toted as an antispasmodic, antiheumatic, hepatic, diaphoretic, and reduces nausea during pregnancy. | |
 |
Licorice Root: Licorice root is an adaptogen and tonic for the respiratory and immune systems. Licorice root helps regulate the hypothalamic-pituitary-adrenal axis. It helps the body to handle stress by normalizing blood sugar levels as well as adrenal glands, and stimulates cranial and cerebrospinal fluid. Licorice root boosts energy, calms the mind and is soothing to the body. |
TONIC:
 |
Red Clover: Red clover is a digestive tonic and a skin nervine herb. Red clover contains a natural plant estrogen called phytoestrogen. Phytoestrogens maintain proper skin and bone health. If ingested it cleanses the blood and detoxifies the tissues. Additional estrogen in the body can alleviate high stress symptoms and reduce cholesterol. | |
 |
Chamomile: Chamomile is a digestive tonic and sedative nervine herb. It was originally used to reduce fevers. Now it has been proven to be one of the safest herbs on the market for relaxation and calming effects. Chamomile has a restorative effect on the body by enhancing the metabolism, treating a nervous stomach and depressing the central nervous system. As a tranquilizer, chamomile enhances sleep and feelings of relaxation. Its properties include anti-inflammatory, anti anxiety, antihistamine, antioxidant and antispasmodic. | |
 |
Skullcap: Skullcap is a tonic and nervine herb that can be used for relaxation without a sedative effect. Skullcap is the best nourishing tonic for the nervous system. It strengthens and supports the nervous system. It slows down the nerves to calm and sooth the body and brain. Skullcap is great for muscles spasms, headaches, agitation, anxiety, insomnia, hysteria, exhaustion, depression and nervous tension. As an anti-inflammatory, and antispasmodic it decreases fevers, enhances digestion, and stimulates liver function. | |
 |
Motherwort: Motherwort works on the circulatory, respiratory, reproductive, and nervous systems as a tonic and nervine herb. Motherwort stimulates circulation to strengthen the heart. It quiets the nerves, promotes relaxation, and relieves stress. | |
 |
Lemon Balm: Lemon balm is a sedative nervine and tonic herb that calms and regulates the nervous system. By inhaling the aroma of lemon balm you will reduce your blood pressure, calm palpitations, reduce rapid breathing, decrease digestive spasms, eliminate nausea and indigestion, relieve migraines and combat fever. It relieves anxiety, dispels sadness, and uplifts the spirit. Lemon balm also has antibacterial, antiviral and antihistamine characteristics. |
NERVINE:
 |
Kava Kava: Kava Kava is a nervine herb from Melanesia. Kava Kava treats anxiety and depression, relieves stress and insomnia. It also doubles as a powerful muscle relaxer, tranquilizer and analgesic, although it is not addictive. Kava Kava works subtly to relax the entire body. | |
 |
Hops: Hops is a nervine herb that acts as a sedative. Its has a calming and relaxing effect on the Central nervous system to ease restless tension, irritability, nervous system disorders, indigestion, and insomnia. | |
 |
Passion Flower: Passion flower has a mild tranquilized effect as a sedative nervine herb. It relaxes blood vessel spasms, decreases migraines, promotes sleep, treats anxiety, insomnia, depression, and nervousness. Passion flower has a calming effect without feeling like one is sedated. This herb calms the body and also is effective as a painkiller. | |
 |
Lavender-Lavender: is known to be the most calming herb today. Just smelling this herb can relax the mind and body by reducing irritability, anxiety, stress and tension. Lavender is a nervine herb with powerful sedative capabilities to promote relaxation, enhance sleep, balance hormones, relax muscles, and stimulate the immune system. It also has healing benefits as a digestive aid. Lavender decreases the stress hormone cortisol levels to slow the brain waves, which reduces stress, nervousness, agitation and promotes a sense of calm. | |
 |
Valerian: Valerian is a sedative nervine used to relax the nervous system. Its ingredients are comparable to prescription grade sedatives given out by physicians. Valerian decreases stress levels, alleviates anxiety, improves sleep, calms nerves, and decreases tension and irritability. Valerian is ideal for those who also suffer from nervous muscle spasm. | |
 |
Oats (Avena Sativa): Oats or wild oats are a functional nervine that nourishes the nervous system. This herb can alleviate mild depression, balance sugar levels, help nervous exhaustion and weakness and relieves stress. As an anti-inflammatory and high in mineral content, oats sooth inflamed skin and strengthen the nervous system. Sarah Labdar, "Herbs That Can Reduce Stress, Anxiety, & Tension", Everyday Health |
Yoga Poses for the Nervous System
Yoga teaches you to calm as well as stimulate your nervous system so as to enable it to reach a state of equanimity. This is achieved through the practice of asanas (Yoga poses), Pranayamas (breathing exercises), psycho-physiological practices such as relaxation and meditation. Then there are the positive attitudes Yoga helps cultivate, thereby establishing complete control over the nervous system. So, in addition to the beneficial physical effects of Yoga are the fantastic, subtle benefits it showers upon the mind and heart. However, this does call for dedicated and regular practice. Some of the asanas that best benefit the nervous system and promote mental and emotional health include:
Inverted poses such as:
 |
Viparita Karani (Legs up the wall pose) | |
 |
Sarvangasana (Shoulderstand) | |
 |
Halasana (Plow Pose) |
Restorative poses such as
 |
Adho Mukha Svanasana (Downward Facing Dog Pose) | |
 |
Supta Virasana (Reclining Hero Pose) | |
 |
Supta Padangusthasana (Reclining Big Toe Pose) | |
 |
Supta Baddha Konasana (Reclining Bound Angle Pose) | |
 |
Balasana (Child’s Pose) | |
 |
Ananda Balasana (Happy Child’s Pose) |
Relaxation poses such as
 |
Dhrdasana (Sideways Relaxation Pose) | |
 |
Nispanda Bhava (Unmoving Observation) | |
 |
Shavasana (Corpse Pose) |
Together with these, it is even better to practice the following Pranayamas (breathing exercises):
 |
Kapalabhati (Skull Cleansing) | |
 |
Anuloma-Viloma (Alternate Nostril Breathing) | |
 |
Ujjayi (Ocean Breath) |
It is even better to take time off to practice a few minutes of meditation and abide by a Yogic diet. This means Sattvic fare (light, pure and predominantly vegetarian). Within three or four months, even the most agitated, anxious, nervous and restless person is bound to see positive results. Whether you practice Yoga to reduce muscular tension, slow your breathing and heart rate, or to calm your racing mind, a simple routine will prove to be the safest and most effective way to a healthier body and nervous system.
Our Recommended Products











